Self-help in understanding the painful big toe joint
This article dusts away some of those myths by discussing the value and benefit of the bunion corrector. I will look at the evidence, and try to remove the technical stuff for the lay reader, without too much scientific indulgence. Nonetheless, we still have to follow the science! Professional advice is still recommended.

The hallux valgus is more defined on the right side but the pain does not always come from the deformity but from within the joint
The Night Splint
Patients often ask if this type of device is of value for their bunion, which does not mean the bump, but the deformity called hallux valgus. The splint actually has a purpose and function and could be valuable, but we have to specify some reservations because at best, it takes time for a painful joint to settle. The big toe (hallux) splint is often called a ‘night splint’ (illustrated as the main image) implying that it can only be worn at night. In reality, many designs can be used during the day but the one I intend to introduce is used as an adjunct to treatment and in some cases exercises.
Hallux valgus (bunion)
There are two important facts regarding hallux valgus; (1) it is very common, mainly found in women, and (2) the deformity cannot be corrected by anything other than surgery. However, surgery is not always required; many agree it should be left alone if the bunion offers no trouble. The only problem lies with the aesthetic appearance. The desire to have a straight toe is important to some. For those who want to know more about surgery or what actions to take, ConsultingFootPain has plenty of information on the subject.
Published in 2019 this book looks at several patient journeys
The Importance of the joint lining
If we ignore the toe’s position and turn our focus on the joint, then the ‘splint’ offers some assistance.
Pain is one of the main reasons that patients seek advice and treatment. It is probably true that as foot surgeons we identify with surgery as the main reason to engage in surgical treatment, purely because of that fact; you cannot correct what is a bone-associated deformity with exercise and externally applied methods – from taping to the insertion of orthoses.
False promises!
This might come as a bitter blow to those who write self-help books, which are, in many ways, misleading and self-gratifying publications of nonsense persuading people to part with money based on false promises!
A joint has two ends covered in cartilage. We now know that cartilage damage in the big toe joint does not mean that surgery is required or that pain arising from a joint depends upon damaged cartilage damage in hallux valgus. Cartilage is important for smooth gliding movements but it can withstand more damage than we realise.
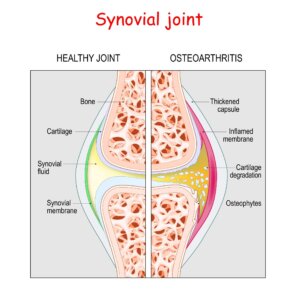
The joint has a cover called a capsule. Inside that capsule, a lining produces the all-important fluid that brings nourishment to the joint and cartilage. That lining also has a rich blood supply. If the lining (synovium) swells, it adds synovial fluid to the joint which does less well. If blood arises within the joint, it forms mini clots that scar the joint and reduce movement. Normal joint fluid is clear and thin. An abnormal joint fluid changes colour and thickens, so is more viscous. Nerves that supply the joint tell the brain the joint is swollen and painful. Nerves also tell the small muscles to tighten up, resulting in involuntary spasms that cause pain and limit joint movement as it stiffens. Of course, some of this stiffening is part of the protective mechanism. We can aim treatment at the inflamed tissue which in turn can help resolve joint pain.
The solution to pain
If we stop the joint moving, we stop the pain.
Therein lies the tale: how long do we stop the movement for, or put another way, immobilise the joint?
 The answer – until the swelling reduces, pain eases and the effect of inflammation ebbs away. We can use pain medication or perhaps anti-inflammatory pain relief such as ibuprofen. Ice is excellent and is used for 10 minutes several times a day. The toe could be strapped, but that is only wise if the swelling is on the way down, not the way up. Pain medication is only wise for short, sharp periods, measured in hours or days. The reason is that pain control does not rest the joint but allows us more activity that may not be ideal. In some ways, we need the pain to inform us not to be silly after injury.
The answer – until the swelling reduces, pain eases and the effect of inflammation ebbs away. We can use pain medication or perhaps anti-inflammatory pain relief such as ibuprofen. Ice is excellent and is used for 10 minutes several times a day. The toe could be strapped, but that is only wise if the swelling is on the way down, not the way up. Pain medication is only wise for short, sharp periods, measured in hours or days. The reason is that pain control does not rest the joint but allows us more activity that may not be ideal. In some ways, we need the pain to inform us not to be silly after injury.
The above scenario is called ‘acute’; as the joint settles, it either recovers completely or becomes ‘chronic’. This implies that a time relationship is applied to how long something hurts. ‘Chronic’ means something has been present for weeks or months without improvement.
Advice & self-help
No self-respecting clinician will tell you to keep treating something that does not improve. Dishing out ibuprofen so loved by the GP should not be used for unresolved or unmonitored long periods. You need to see a foot expert, a podiatrist or a foot orthopaedic surgeon. Physiotherapists, osteopaths and chiropractors might assist but the real understanding comes from a full-time knowledge of podiatric (foot) medicine. Helping your bunion yourself
Where does the bunion corrector splint come in?
Forget the soft neoprene or latex splints that promise correction of the bunion although they might be better than nothing. We need to look for something a little firmer, perhaps something with a plastic skeleton and something that is adjustable. Sadly all the products found online will use the word ‘correct’ – this is not going to happen, but what will arise is the result of calming down the joint allowing it to settle. This is the route I am advising. Use the splint to help recovery. Strapping the toe can be useful but for short periods because of skin irritation. See my video on strapping to limit movement.
Building evidence for the toe splint
In each case, only the first person named on each reference paper is used although each study was co-authored (see the references). If you’re like me, I tend to ignore anyone after the second author as scientists like to latch on to expand their literary prowess.
Night splint & insole
In Tehran, Ali Tehraninasar looked at 30 female patients aged 19-45 (2008). The research divided the women into 2 groups – one group wore an insole with a toe separator, the other group a night splint. The period of follow-up was 3 months. The pain was measured by intensity, a reference we call a visual analogue scale (VAS) – where the patient marks a 10cm line so as pain is more intense, the mark is closer to the 10cm end than the 0cm end.

the visual analogue pain scale is often used as a numerical scale of 1 to 5 or 1 to 10. The researcher used a 10 cm line
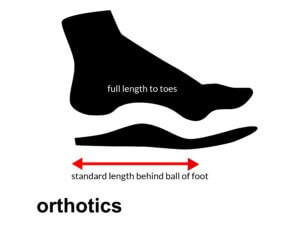
Tehraninasar found the insole and toe separator had a better effect than the night splint when controlling pain. The insole was semi-rigid and ended behind the ball of the foot (metatarsals). The person who made these devices was an orthotist and each device was taken from a cast. Because the material used in the design took up more room, an extra +1 shoe size was necessary. The night splint comprised mouldable foam and a rigid polyethylene bar.
Manipulation and night splint
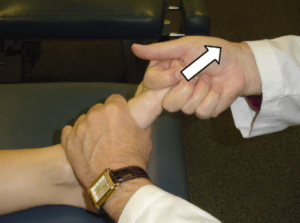
manipulation includes distracting the joint, a useful technique for freeing up scar tissue and resistance if the joint is not rigid
Morne du Plessis published his paper in 2011. This was a joint effort between South Africa, the USA and Australian contributors in chiropractic. Again a night splint was used as a rigid design (illustrated below). The numbers in the study are the same as Tehraninasar’s cohort – 30 divided into two groups. In this case, the difference was the manipulation exercises used in one group with a night splint, and the other without.

night splint used by du Plessis. This is a fixed system and an example of a semi-rigid splint unsuitable for closed in shoes
Du Plessis described the deformity as having mild to moderate pain. In this paper, the researchers used the VAS method of assessing pain and a marked questionnaire (Foot Function Index) scheme before and after. This would give them a score or value. Ideally, the score after treatment is lower than at the start of treatment. Additionally movement was measured. Three measurement criteria are better than one. The follow-up period was a month and manipulation added.
The night splint and manipulation proved more successful than doing nothing. The authors believed such observations could lead to the consideration of using the manual manipulation technique and night splint before surgery.
Dynamic splint
Christian Plaass published their paper in 2018 and is the most recent of these 3 studies. Again the study focused on symptomatic hallux valgus. A total of 55 patients were used in two study groups: 26 and 29 respectively. The period of follow-up as with Tehranansar was 3 months. Unlike the other 2 studies, this was a German team of orthopaedic surgeons. The detail of the state of the joint was thoroughly documented. No degenerate patient was allowed in the study – the joint had no cartilage damage or bone changes. Unlike the other studies, a control was added. This meant that 26 patients had no treatment during the same period, while 29 were all issued with the designated Halluxsan splint (illustrated). The conclusion as one might expect, those with the dynamic splint did better than those left without treatment. In all cases, there was no change in the angle of deformity so the joint did not change in position. Pain however was minimised and delayed further treatment.

commercial night splint with adjustable traction on the toe. Free up and down movement was allowed – Halluxscan
The clinician dilemma
The evidence shows that studies do not have large numbers of people, making conclusions more difficult than if large study numbers could be recruited. However, small numbers are a reality in orthopaedic work. All studies show that deformity cannot be altered but symptoms can. Taping to the skin cannot be used indefinitely because of damage to the skin. Splints designed along the lines of the Halluxscan make sense as it is adjustable for tension making them distinctly different from Du Plessis’ splint. The splint or as Plaass describes,
“allows for a prolonged stretch to correct contracted tissue and influence the H.V (hallux valgus angle) position. All patients in the treatment group were instructed to set the adjustable Quengel mechanism, such that there was no perceptible traction, and to wear the brace during their rest time for as long as tolerated.”
The Quengel mechanism is simply a tensioner mechanism pulling the big toe away from the second toe.
Will the patient listen to the clinician?
In many cases, impatient people want a quick fix!
Pain and inflammation following injury take as long as it takes. Surgery is not the first-line answer unless the bone and joint have actually split.
You can buy the equivalent night splint online

an enlarged view to show tensioner and cable
Conclusion
Evidence shows that improvement can be achieved using the study period from 1-3 months. There is a suggestion that after this, some patients may have other interventions, including injections and surgery.
The reader presenting with a painful bunion should always seek a foot specialist, a podiatrist or an orthopaedic foot specialist. (Note not all orthopaedic surgeons specialise in feet). Planned care could include this mechanism. The author has found several similar mechanisms to the Halluxscan purchasable online (see above). Not all splints offer tensioners and have a moving mechanism to allow up and downward movement. The price is the giveaway and the mechanism that ConsultingFootPain purchased to study the splint comes in at £30-50 (2022). Lower prices splints are unlikely to have the tensioner.
ConsultingFootPain cannot suggest the splint will suit everyone, but it affords rest to inflamed joints once the swelling reduces. Clinical examination using imaging is often recommended to establish if damage has arisen. Spasm should be ruled out but for 3 months following any internal joint inflammation is a useful adjunct to management and should be considered before surgery as an option.
![]()
Tehraninasar, A, Saeedi, H, Forogh, B, Bahramizadeh, M, Keyhani, MR. Effects of insole with toe-separator and night splint on patients with painful hallux valgus: a comparative study. Prosthetics & Orthotics Int. 2008;32(1):79-83
Du Plessis, M, Zipfel, B, Brantingham,J, Parkin-Smith, GF, Birdsey, P, Globe, G, Cassa, TK. Manual and manipulative therapy compared to night splint symptomatic hallux abducto-valgus: An exploratory randomised clinical trial. The Foot. 21(2011) 71-78
Plaass, C, Karch, A, Koch, A, Widederhoeft, V, Ettinger, S, Classen,L, Daniilidis, K, Yao, D, Stukenborg-Colsman, C. Short-term results of dynamic splinting for hallux valgus –A prospective randomized study. Foot and Ankle Surgery 2020; 26 (2):146-150
Thanks for reading The Bunion Corrector. Helpful or Not? by David R Tollafield
Thanks for using ConsultingFootPain. The author is a former podiatric surgeon. You can find other articles on this site for professionals and lay readers.
Published by Busypencilcase Communications. Est. 2015


Trackbacks/Pingbacks