Pain after injections for nail surgery
Pain after injections for nail surgery is brought this month to readers by Alison Charlton. Alison is an avid reader of Podiatric Reflective Newsfeed and publishes her short case history for ConsultingFootPain. Many queries are being raised on Podiatry Forums covering nail surgery. If you have a case to share or query, you can write to ConsultingFootPain. (Editor)
Presentation and Complaint

Mycotic nail causing deformation. This is only a typical example.
A 42-year-old female attended the clinic for the removal of her heavily mycotic nail (the illustration is not the patient). The nail was causing discomfort due to its thickness. She was taking no medication, had no allergies, and had normal vascular and neurological tests. She is a keen runner, running many marathons and averaging 30 km weekly. She is a busy mum with two children.

https://www.dreamstime.com/photos-images/signing-consent.html
Consent & Procedure
After lengthy discussions and outlining treatment options, she chose to have a TNA with phenol. The injection was from one side using the ring block method (see method below). The nail avulsion was uneventful, although the nail bed required more scraping than normal to clear it.
Post-treatment sequela
The wound healed within four weeks. At 5 weeks post-op’ she then contacted the clinic to say she was still experiencing pain at night at the injection site. The pain was only manageable with paracetamol. She attended the clinic, and I checked her sensory nerve sensations again, particularly light touch, which was normal. She described the pain as ‘burning’ and only occurred at night. She insisted that the pain was at the injection site and not around the nail area. She had started running again, approximately 5km on alternate days.
Advice and follow-up
I asked her to restrict her running to give the area a chance to settle and discussed her case with a consultant colleague. It was agreed to desensitise the area 2-3 times daily by deep massage around the injection site with standard skin cream. If possible, the mechanical massage could be supplemented with an anti-inflammatory gel when it became sore instead of paracetamol. Products such as Ibuleve, Voltarol or Feldene were available to the patient through OTC/pharmacy sales. The patient was reassured to hear that although unusual, this was not abnormal. Because this was not an expected outcome, it had not been highlighted before the surgery commenced. Within two weeks, the patient reported no more discomfort overnight and a complete resolution to the situation. She is again training for her marathon.
Reflection

Footwear
As a keen runner, this lady appeared to have high expectations, with a rapid return to running again soon after her procedure. I did not see the trainers she used for running, but those she wore to the clinic were fine. Running footwear should have been checked as it may have exacerbated the problem. If there had been no resolution, this would have been an essential next step.
Hypodermic needle
A needle close to the phalanx can lead to discomfort, although 5 weeks is longer than usual, which is not unheard of. Post-injection neuralgia can occur, although there is little reported evidence. Most injections leave discomfort for a short period of 2 days to 2 weeks. The worst-case scenario would be a low-grade reflex pain syndrome. In Complex Regional Pain Syndrome (CRPS), the resulting pain and the initial injury do not correlate [1].
Pathogenesis
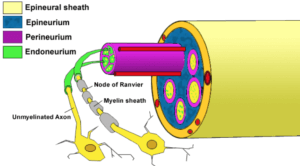
In this particular case, nerve axon (illustrated) irritation with swelling and haematoma were the most likely causes. While resolution was fairly rapid in this case, we are reminded that nerve damage can take 6-9 months to settle. Local periostitis due to the needle scraping the periosteum was also a possible cause and could have lead to bruising and sensitivity. Another possibility was a local abscess, but most likely, this would have been apparent before 5 weeks post-surgery. Additionally, infection was unlikely based on presentation, colour, swelling and low-grade discomfort. A medial-oblique and lateral x-ray of the toe would aid with this diagnosis.
Reflection
 Information is scanty on digital block injections. Säkkinen, J et al 2005 [2] points out that post injection neuralgia is rare. We can deduce that dental awareness is far greater than in podiatry.
Information is scanty on digital block injections. Säkkinen, J et al 2005 [2] points out that post injection neuralgia is rare. We can deduce that dental awareness is far greater than in podiatry.
“Paresthesia or neuralgia is usually transient, but may be permanent if anaesthetic solution is injected directly into the nerve. Therefore, injection against pressure must be avoided. Actually, it is very difficult to inject into a nerve because of the tight epineurium. Instead of that, when the needle has transfixed the lingual nerve after injection and is withdrawn through the nerve, a little amount of anaesthetic into the lumen and onto the needle can cause a chemical damage.”
Metcalfe & Riley (2010) [3] published the latest definitive book on local anaesthetic foot and ankle techniques. The authors state;
“…even with excellent technique and application of nerve stimulators, it is not always possible to avoid accidental intraneural needle placement… Whilst other techniques may result in accidental ‘needle paraesthesia’ this is quite different from deliberately setting out to create it when we know there is an increased potential for intraneural injection.”
Fortunately, my patient’s case was resolved quickly. An abscess was ruled out and would likely have shown up in a shorter time frame. A low-grade reflex sensitivity or bruising due to periosteal irritation of the phalanx was possible. The follow-up appointments were part of the procedural package as part of good practice. It is hoped that this case history will assist both patients and colleagues by sharing relatively poorly reported sequela in the literature. Management was maintained at a conservative level with reassurance. Discussing problems with experienced colleagues is important to ensure a proportional and balanced approach is considered. Perhaps local sensitivity is more common than we admit and remains unrecorded.
[1] Srinivasa N.Raja, Theodore S. Grabow; Complex Regional Pain Syndrome (Reflex Sympathetic Dystrophy). Anaesthesiology 2002; 96:1254-1260.
[2] Säkkinen,J, Huppunen, M, Suuronen,R Complications following local anaesthesia. Tannlegeforen Tid 2005; 115: 48–52
[3] Metcalfe, S, Reilly, I Foot and Ankle Injection Techniques. A Practical Guide. Churchill Livingstone/Elsevier.pp67-68
Thanks for reading ‘Pain after Injections for Nail Surgery’ by Alison Charlton
Published by Busypencilcase Reflective Communications Est. 2015

Submitted February 2021 and published 1st April 2021. Updated 10th June 2024.


I had my big toe nails removed 6 months ago and had two infections and burning pain for 4 weeks. I was put on antibiotics and strong painkillers.
My nails on the sides have back again and I cannot wear full shoes as the pressure on my toes is unbearably painful. I am now having red light /(cold laser) treatment for the next 3 weeks and iam hoping this stops the pain.
I am sorry to hear about your problem Elisabeth. At six months, full recovery should be expected. Unfortunately, regrowth is a problem. You don’t say how the nail was treated – surgical excision or chemical – so I cannot offer too much advice on the specifics of treatment. I hope you find relief from the laser treatment but if not then let me know. Confidential discussion can be provided via busypencilcasecfp@gmail.com – David
Please tell me if this works. I still have pain
after 2 years in my toe from a toe nail avulsion. Part of my toe nail was removed.
Can you let us have more information about your foot problem? Why you had an avulsion and the procedure. You can write to busypencilcasecfp@gmail.com, attaching photos if this is available. David
I had my big toe nail removed,after numerous attempts to cut out the ingrowing nail,my big toe was injected,and a gadget placed around toe joint to prevent blood flow,toe nail removed,and since that day my big toe is constantly red,and the back of my toe is partly numb,a piece of my nail has regrow
Dear Paul, it might surprise you that more people experience this than data officially records. The gadget, of course, was a tourniquet to ensure blood did not affect the surgical field. Most nail surgery uses phenol, a caustic based on carbolic acid, the antiseptic used in Lister’s preparation. It destroys protein and the nail matrix. Concentration is critical to the success of treatment. Now the giveaway here is the constant redness in the toe.
In some cases the skin (tissue) reacts abnormally and remains blemished. The numbness is less common and suggests damaged nerve endings as in neurolysis. You don’t give a timeline so I cannot make any comment about how long this may last for. I hope this helps.
I had an ingrown toenail section excised with the chemical applied at the nail bed to stop regrowth, 4 and a half months ago. It resolved successfully, however since that time I continue to experience pain within my toe. I can press all around the operated area and it’s not tender. Daily, Intermittent pain generates from inside my toe. That’s the only way I can describe it. I can only assume there was nerve damage from the anaesthetic injection and I wonder how long it will persist. I’ve had a similar experience with a dental injection, affecting sensation in my tongue, which happened 24 months ago and is not quite resolved yet.
Dear Jackie, thanks for your question. I am glad the nail section has been resolved. Your problem is not unusual and probably poorly reported. I cannot comment on the dental side of your treatment, but tingling or local changes, including numbness, usually follow nerve damage. The nerve can be bruised when local injections are given, but it is rare for serious damage because the clinician will recognise nerve penetration and pull back. Local injections for ingrown toenails are not performed under guided control as the nerves are very small. Bruising and irritation of the outer sheath are reversible but can take up to 9 months to settle. Localised massage and using an anti-bruising agent, Arnica or Hirudoid gel, may be of some value. If matters don’t settle or become more intrusive, do seek a second opinion. Please let consultingpain know how you get on. David
Thanks David. I do wonder if having fibromyalgia impacts my pain perception once a nerve is damaged also, perhaps more than someone without fibromyalgia.
When the shot was administered, the clinician would not have known a nerve was involved as I felt an uncomfortable sharp zapping pain but presumed that was my normal reaction to a shot and just breathed through it! I will try localised massage for sure. At this point, I recognise that the nature of this pain will probably take some months to fade away.
Thanks for taking an interest and giving your opinion.
A reply has been sent to the reader and not published.
I had a part of my toenail excised years ago, and it still feels bruised as the needle injection site.
Reply from David – this is a rare post-operative condition and sounds nerve related but without further details it is always difficult to comment Sam.
I had a partial nail avulsion 2.5 months ago by a very experienced Podiatrist. The nail has healed but the side of the avulsion is red. Its not tender to the touch now but it used to be hypersensitive to touch during the initial healing process. Now I just feel pain from inside the toe near the front edge of the toe and it seems to radiate up into the top of my foot sometimes. Some days I don’t feel it that much but other days I feel it alot. When I soak in in ice water it numbs it up and I think it calms the nerve down for a few days after. Then it seems to slowly return. Do you think this will eventually resolve?
Dear Brian, given your description I am sure it will settle. There is never a specific recovery time and I believe 2 1/2 months is still quite early. Thanks for sharing this information. David
Its been 3 months now and it seems the sensitive within the toe is now hypersensitive towards the top of my foot going to the inside of the ankle. So the tighter the shoe I wear the more painful it becomes. Is this still due to the nerve in the toe? In summary it seems like the hypersensitivity is transient. Is this reported by others?
Hi Brian, footwear will always be a problem where compression arises. As you have described, possible symptoms that reflect backwards, and your podiatrist is very experienced (Jan.2023), I would direct you back to your clinician purely as this type of concern does require an examination with some specific local sensory testiong. I feel my own comments may not be that helpful. I am sorry not to be able you any definitive advice. David
My great toenail was removed 4 weeks ago. I am having severe burning pain at night. Even with painkiller still painful. I took antibiotic for one week. Why my toe have burning pain at night. Mostly tip of my toe hurts more at night.
Sara, did you have a chemical applied, nothing – just removal, or was this surgery performed with stitches afterwards? David
I had an ingrown toenail, removed from the side walls of my toe back in November. After a couple months of healing, and noticing that it was not completely drying out or scabbing up, I went back to my podiatrist, to discover that I had developed a granuloma. I had the procedure to have the granuloma removed back in the last week of January. Of course, there were more injections done during this procedure and I am still experiencing pain. The pain, however, isn’t completely at the sight of the granuloma. It’s more so closer to the free edge of my toenail. There is no bruising, swelling or discoloration however, it is sensitive to the touch and with wearing certain shoes. Could this be due to nerve damage at the injection site?
Dear Marie, thank you for your reply. Granulomas can form as a result of a defective healing process. They are made up of poor-quality blood vessels and bleed easily. I assume that you had a phenolisation of the nail sulci in November. You may have seen my comments from previous queries. First, do I think you have nerve damage? We need to define nerve damage as most interventions damage nerves, but they repair just fine. There are nerve concerns that take longer to heal, and this leads to a confused state. Honestly, it is not easy for any clinician to judge the extent of the nerves as they are small, but nerve endings in toes are very sensitive as they include pressure sensory nerves. ‘Give it time’ and ‘it will settle in the end’ – may appear frustrating for patients as a comment, especially if there is no emotional sensitivity. As clinicians, we are not always good at making comments sufficiently contrite. A free edge is a sensitive place as well.
Here is what you must do. If the pain is constant, you need pain medication or you cannot continue your role, seek advice from the person treating you. If you can cope and do not have the impact suggested above, you must bide your time. I don’t have statistics on post-injection pain incidence, but first, I think it is more common than we think. Secondly, some of these pains take 3-6 months to settle as the nerve alters its structure and physical chemistry while settling. A rule of thumb has always been that if, after 9 months, nerves remain abnormal, it is permanent. Take some assurance; I suggest this is less likely in your case. David
Hey David,
I got my ingrown toenail remove both sides 2.5 months ago.
I had all closed up and looks good except it is red on both sides and below.
It is also sensitive, I went back and they couldn’t diagnose it.
Would you have any ideas?
Thanks.
Hi Daniel, further to your enquiry. Could you send me a picture of the toe in good light and resolution to busypencilcasecfp@gmail.com, and I will see if I can provide a viewpoint? Can I assume this was a chemical treatment?
Hi Daniel
Thanks for the photo which was helpful.
The nail has the appearance of a recent chemical destruction on both sides which has left the sides slightly splintered. That is quite normal but would need careful filing and trimming. I have never known it to be a big problem longer term.
I cannot see any significant inflammation but you may wish to soften the sides with creams such as an antiseptic under a plaster for 24-48 hours to see if this helps. Sensitivity is not unusual for a while and I probably would suggest 3-6 months, but it should diminish. Check footwear of course and that is not a source, but see it you can file the edges smoother to remove sharpness. Of course following any procedure the clinician does have a duty to follow up any concerns should you remain worried.
David
I had some of the toenail removed from my right big toe on both sides due to in grown toenail about 2 years ago. I still have pain at the base of the nail on the left medial side. My podiatrist said that I may have to live with it. I sometimes have a hard time sleeping with this annoying pain. He said to try Voltaren. But is there anything else I can do to stop this pain? My doctor said the nail is not ingrown so performing surgery again will not help. Do you think cortisone injections will help? Do you have any suggestions that will help?
Charles, I rarely say this on my site, but consider a second opinion in the first case just to widen your options. I would be concerned you being prescribed Voltaren for any length. Dvaid
I had a partial nail avulsion six days ago. Everything went and felt fine but yesterday I started having burning and tingling pain around the injection site – up into the top of my foot and ankle as well as my leg. The injection site now looks more like a bee sting where it didn’t before. It sounds like from other comments I don’t have anything to worry about and should just give it time but, should I reach out to my doctor before my scheduled follow up just to be sure?
Time is the best healer but do ask your doctor Stacey if you have concerns as problems should be registered and doing this later is less ideal. David
Hi David Tollafield,
Would I be able to get your opinion on my current situation/treatment by emailing you at busypencilcasecfp@gmail.com? I’m akin to the others here where I had a badly ingrown toenail removed, this started 6 years ago and it would return annually (even after phenolisation), nerve type pain lingers to this day with some speculation of mild CRPS as mentioned in this article.
Regards,
Chris
Yes Chris I am happy to look at the story. David
Thank you David, email sent with subject line “ConsultingFootPain – Chris on April 21, 2023 at 12:39 pm”
Hello David,
I had my big toenail totally removed two weeks ago. I did not feel pain the first week, but I’ve been feeling so much pain for the past 1 week now especially around the joint of the toe.
The pain radiates to the back of the toe & it hurts so much that I can barely move the foot sometimes.
Although, I’ve been suffering from nerve pain before the surgery but that’s majorly from the tip & a portion of the left of the toe. Now I’m suffering from what seem like joint pain and sharp shooting pain that radiates to the back of the toe. What could be the cause?
I’m currently placed on neurovite forte and Pregabalin capsules by the way.
Thanks for writing in Anna. I am sorry to hear about your problem. If you have been prescribed Pregabalin then I assume you are under a doctor and that infection has been ruled out. Nail surgery often uses a chemical. Can you describe your treatment as this may be the root cause. As these messages are published on the internet you may wish to communicate privately with me through busypencilcasecfp@gmail.com
David
After having complete nail removal from my great toe.. over 2 weeks later I am still experiencing nerve pain from the injection site… currently on several types of medication.
The pain is like toothache in your toe, the pain is awful
Sorry to hear about your post op nail problems Scott.
Can you say more about your surgery. Was this just under local anaesthetic? Did it have an infection to start with? What pain management were you advised? Did you have post operative information. Readers can understand more about the problem and I may be able to reply more helpfully.