Defining the hard skin problem on feet
While we regard hard skin on our feet as unsightly, for most people, hard skin relates to areas that have contact pressure. Areas that do not directly take a bearing, often called loading, may be due to other conditions framed around dermatological, medical conditions such as psoriasis, ichthyosis even fungal infection. The skin over the knee may thicken due to an occupation where kneeling is common, but this is often hidden from sight. Congenital hard skin hyperkeratosis is alarming and can cover wider areas than the sole (plantar) and hands (palmar).
“A condition marked by thickening of the outer layer of the skin, which is made of keratin (a tough, protective protein). It can result from normal use (corns, calluses), chronic inflammation (eczema), or genetic disorders (X-linked ichthyosis, ichthyosis Vulgaris).” https://www.cancer.gov/publications/dictionaries/cancer-terms/def/hyperkeratosis

Physiological callus developed days after 2 days of walking around a European city – author
Physiology effects
If you play racquetball, dig your garden over with a spade or fork, or use a screwdriver or paint brush on virgin skin, the surface reddens and forms a soft swelling associated with cellular fluid. This frictional effect excites inflammation, and the skin adapts and responds by thickening, usually where the blistering effect has not lost the covering roof. This is known as a physiological callus. You stimulate a part of the skin that does not usually experience pressure, and suddenly within days, the skin has thickened after the redness subsides. After a while, if the stimulus disappears, the hard skin returns back to normal. The colour is pink rather than a yellow-brown hue. The flexibility (elasticity) returns, and all is well. This is known as a feedback system in the body at the skin level.
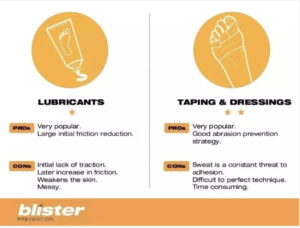
If you cover the area before the redness arises, either using gloves in the case of manual work with hands or using a blister plaster before a sporting activity, blisters and hence hard skin are minimised.
Tipsfortrips accessed October 2022
Podiatrists taught to use scissors as part of their practical skills can develop a thick nodule of skin around the finger, rather than the thumb. This remains permanent all the while scissors are used daily and disappears with reduced scissor activity. Guitarists learn to harden the tips of their fingers. In both cases, once the skin adapts usefully, any discomfort or blistering ceases. There was a well-known practice for hikers to use surgical spirit days or weeks before embarking on long walks. The spirit would dry the skin, causing it to harden and reduce blisters. This little tip is no longer in vogue, with more practical advice offered to would-be ramblers. Here is the link for tips https://fitfortrips.com/how-to-prevent-foot-blisters-while-hiking-and-walking/
Factors influencing hard skin formation
(diagram Websters https://webstershoes.co.uk/fitting-guide)
Footwear purchase
There was a well-known saying – ‘you need to break your shoes in slowly.’ This means when buying shoes, expect to take time to adjust to comfort. This is not only nonsense but implies the shoes do not fit correctly. While many shoe shops are keen to measure children’s feet carefully for girth (fatness) and length to ensure growing room, such care does not always exist for adults. The width which allows narrow to wide feet, and thin to fat feet to be accommodated is classified as narrow A to wide E . The very narrow shoes may have C to wide EEE as in the case of Hotter (see table). Of course, if your shoe does not come with the advantage of half sizes and width options, it would be better not to make any purchase rather than suffer.

Shoe stretchers can be purchased for under £20 online and prevent tight areas from deformed areas from rubbing. It is always best to select unlined leather which stretches without the pain of having to ‘break shoes in’.
If your foot is not conventional in shape, and you have bone prominences, the chances are these parts of the foot will be exposed to pressure. You may have to measure the largest foot and fit this, then use an insock (filler) to allow the smaller foot a better fit. Most shoe shops carry insock fillers. Unlined shoes stretch better than lined shoes; you can push paper or shoe trees into the toe box to stretch the shoe. Professional stretching is less common than once available. Cobblers may offer a service to do this for you, or you can purchase a shoe stretcher for under £20 online.
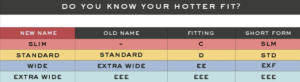
Taken from the Hotter shoe website – October 2022
Gender & environment
Technically, when it comes to hard skin on feet, there is no difference between the genders of biological males and females. However, females tend to suffer in relationships with shoe design. The type of activity, occupation and environment will affect skin changes under the foot. The army medical corps poorly managed a soldier with an enlarged lump on the back of his heel. He developed an infection, and his term of service was shortened, resulting in his suing the Ministry of Defence (UK). As he was one of my cases, I lamented that the British army does not have podiatrists attached to the medical corps as in the USA. The Highways Agency (HA) used a limited range of boots for its road traffic officers. These did not suit some officers with existing foot problems. With the HA, footwear was examined, and wider options were made available to account for foot problems. A manual was written to guide HA regarding foot problems.

As in the soldier’s case history, the heel bump or Haglund retrocalcaneal exostosis is shown

Common foot deformities and bumps, as seen in the Highways Agency case. Quality, well-designed footwear that fits correctly is important
Moisture and humidity play a part, and hard skin becoming infected with bacteria or fungi can cause unpleasant odours and thickening of the skin. Aspergillus sydowii (aspsy) has been shown to form cells, sometimes called Zombie cells that cause hyperkeratosis (Zu, 2019 – see reference at end of article).
Age will change the skin structure with the loss of elasticity, which may come with dryness. Any material that has lost elasticity is less resistant to forces across its surface, so we find human skin on feet can change over the years. Smoking is harmful to circulation and, in turn, affects skin quality.
Infection and skin type
Our DNA makes us unique; the skin on each human foot is not only different in genetic makeup but responds differently to external pressures; for this reason, patient A may have a particular skin type compared to patient B.
Of course, if we throw diseases affecting blood supply and nerve supply into the mix, the effects on the skin change yet again. Pressure causes damage at a deeper level. The biochemistry of skin response to variations is hard to establish. We know much about skin and its chemistry about abnormal genes, but not so for the straightforward occurrence of hard skin. There are those who suffer blisters to a dangerous level of shedding skin due to abnormal skin chemistry (epidermolysis bullosa). Psoriasis causes faster skin cell turnover, and ichthyosis reveals a fish-scale-like surface. Congenital hyperkeratosis can affect the skin in general and not the foot alone.
The detailed structure of the skin can only be simplified in a short article. The surface layer is made from 4-5 intimate cellular layers that change from the lowest level to a thick, resistant top layer made of cells without nuclei. This section of the skin is known collectively as the epidermis. It is separated by an important membrane (epidermo-dermal junction or basal layer) that itself influences much that arises above in the epidermis. Faults at this level also influence skin appearance. The next layer is called the dermis and below this, the hypodermis (fat layer). Keratin, a skin protein acts as a barrier and produces lubrication and sweat. Specialised cells include the Langerhans cells which lie in the upper part of the basal layer. These cells provide an immune function. We can see that skin is both complex and works at a microscopic level offering various functions.
Classification of hard skin
This article has discussed hard skin alone, a condition called ‘callus’. A ‘corn’, once called a ‘clavus’, is an organised area within the skin, more often associated with the surrounding callus. You can refer to Tollafield’s directory of callus to gain a better insight into some of the variations affecting the sole of the forefoot.
In 1983 and 2016, I looked at classifying callus on the sole of the foot. The study involved students at Birmingham and Huddersfield studying podiatry. The first study looked at 1700 patients, the second study used 3 patients. The difference between the studies was the first was not controlled while the second was, hence the smaller numbers of patients, but a larger number of student observers (56).
The hypothesis used in both studies was that there are four types of classification. A general thickening without a defined border (Type 1). Type 2 is well-defined and may have different depths of thickness. Type 1 forms from the physiological description discussed above. Type 3 has small seeds but no distinct callus. The last type, type 4, is the most severe type, where the callus may have variable depth but will have a core area of the nucleus at some point. Type 4 will also relate to the worst type of symptoms.
To classify callus and corns elsewhere on the foot is entirely possible, but to date, it has not been followed up. Painful areas between the toes are often white with a high water content called macerated. This foot area is prone to fungal infection, and the corn formation is often difficult to treat.

Debridement of a type 2 callus with a sharp scalpel in the hands of a professional. In unskilled hands, scalpels can cause significant damage.
Deeper problems of concern
While the skin may cope, the foot throws up a few problems when the bulk of skin develops a long-standing effect; the deeper tissues alter their shape and respond, forming organised changes. One such change is the formation of a cyst or sac, often called a bursa. These changes may be associated more significantly in patients with rheumatoid arthritis, but many patients experience pain under callus without medical concerns.
Patients can easily maintain Type 1 callus using softening creams and pumice stones. However, escalating pain should be taken seriously, as bursae can exist under the skin without thickening.
Type 2 callus is altogether different and may require podiatric assistance or the help of a foot health practitioner. The reason for advice comes from the fact that the skin depth is uneven. The term debridement is the removal of dead or decaying tissue. Deep skin can reveal foreign bodies upon exposure, where particles from hair to splinters have penetrated the skin. The longer such conditions are unexposed, the deeper damage arises from inclusion cysts. Histology taken from biopsy or excision shows an unusually high incidence of viral infection (human papilloma foot virus). Coexisting corns with verrucae fail to clear without professional management. Unfortunately, it is not easy to determine whether a corn has a viral co-infection.
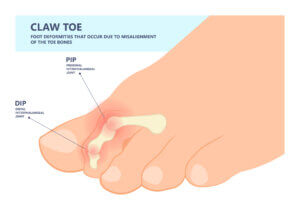
Hammer and claw toes become fixed deformities into adulthood as the joint becomes stiffened with tight tendons and cartilage changes. The skin is exposed to the pressure imposed by the toe box. These knuckle-like joints bear the brunt of blistering, cysts, chilblains and form sinuses ( and organised hole with a tube) that can become organised. Infections of bone are rare but can arise if the individual has poor circulation or is immunocompromised.
Summary
Corns and calluses might be considered minor or cosmetic and need a bit of skin scraping. The truth is that there is a difference between callus types, and corns may manifest due to deeper changes. CFP will be looking at treatment and corn plasters in a further edition.

For the original Tollafield papers, please select publications
Reference
Zhu, C.X., Li, X., Tan, X. et al. Zombie Cells, Composite Cells of Fungal–Human Keratinocytes of Plantar Hyperkeratosis-Like Lesions. Mycopathologia 184, 597–605 (2019). https://doi-org.libaccess.hud.ac.uk/10.1007/s11046-019-00369-0
Thanks for reading ‘Hard Skin on Our Feet’ by David R Tollafield

Why not read the article covering obstinate corns over tendons recently published on this site
David is the editor and author of ConsultingFootPain (CFP) and produces regular health articles dedicated to feet published under Busypencilcase Communications Est. 2015


Recent Comments