Broken bones and feet – an introduction
The theme – does it matter which bone you break? The answer, of course, is a simple yes. But, unfortunately, not all bones heal the same way or are prone as others to damage. As a lay article I hope this updates any previous knowledge, or if you are a clinician a little refresh perhaps? The second matter is what causes a fracture or break? Are these always what they seem? I provide a little bit of physics, chemistry and nutrition to bring into focus the less known aspects behind bones breaks.
When my wife broke a bone in her foot back in October 2021, no one was more surprised than me. During my career, I have been interested in two facts. How people walk on their feet for so long without knowing they have broken a bone. Secondly, the methods we use to make such an assessment can fail, or the diagnosis can be missed. I wanted to introduces broken bones into the discussion about foot health as part of my ongoing pain series. Officially we all know breaks as fractures. Fractures, by dictionary definition (Little Oxford dictionary, 2002), are cracks or breaks which serves my purpose well. A quick check on Wiki and the definition has not changed but our views have.
Whistle stop tour of anatomy
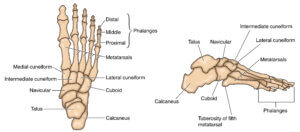
There are 26 bones in the feet plus two small seed-like bones (sesamoids) making 28 constant bones in the foot. The bones are either small bones or long bones. Long bones give the foot shape; width and length. Small bones are more building bricks in the foot and shape the arch. The heel bone is a platform for the leg to sit on and protected by a fat heel pad. The names given to bones are primarily Latin and have changed little over the years, although the ankle bone is now talus but previously known as astragalus. Bones are covered in an outer layer of a hard or compact bone called the cortex. The inside is made of spongy bone, which one might like to think of as ‘aero’ type – after the chocolate bar with air holes. Inside the long bone is a medulla cavity in which marrow sits. Marrow contains fat and blood producing cells, including white cells for immune response.
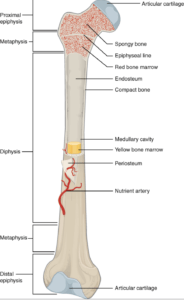
Illustration from Anatomy & Physiology, Connexions Web site. https://en.wikipedia.org/wiki/Long_bone#/media/File:603_Anatomy_of_Long_Bone.jpgJun 19, 2013.
I have used a long bone to show the basic structure in the illustration above. This is the thigh bone or femur but it illustrates all the key features beautifully and the metatarsal long bones follow the same structure. Short bones are often cube-shaped and do not have a medullary cavity. Look at the anatomy of the foot below the table, and we see the following:
| LONG BONES | SHORT BONES |
|
Forefoot: Metatarsal 1-5 Toe end: Phalanges of each toe of which there are three except the big toe |
Mid-foot: navicular, cuneiform x3, cuboid Hindfoot: calcaneus heel bone and ankle bone the talus. Additional bones: 2 sesamoids under the first metatarsal |
Each long bone has a shaft (middle part or diaphysis) and 2 ends, often known as a head and base. As clinicians we use different terms that mean the same thing, e.g. distal, proximal to determine which end we are talking about.
What else do we need to know?
The bone’s cortex has a lining with a blood supply called the periosteum. ‘Peri’ means outside, and ‘osteum’ is bone made of bone cells. The head and base of each long bone has cartilage covering the ends. This is soft and has no blood supply. However, it is smooth and makes up joints. When we grow, we have small areas of cartilage that appear as gaps on x-rays. These are growth sites called epiphyses. When males and females mature around adolescence, these growth sites stop growing and change from cartilage to bone; the gaps now disappear. If you want to know how we determine age in humans, we look at whether the growth sites have closed or are still open on an x-ray. X-rays do not pass through bone, only cartilage and soft tissue like muscle, fat and skin. Some bones have projections into which tendons are attached. The three bones that these affect mainly include the navicular, the base of the fifth metatarsal (called a tuberosity or styloid process), and the back of the heel bone where the large achilles tendon attaches. There are others but not of importance in this introductory discussion. We nearly have everything we need to know about bones before talking about fractures but there are a few more important things we must cover to keep bones healthy.
A bit physics, chemistry and nutrition
Healthy bones are made up of calcium phosphate and a protein called collagen. The outside hard cortex can resist stresses and strains of everyday life. This means compression, tension and shear forces. Mostly these occur as slow, low grade pressures within or against different parts of bone. Long bones in the foot are slightly curved to give spring resistance and are triangular in shape, which makes them very strong. Forces when applied very fast cause far more damage; road traffic impact injuries are an example or even gun shot wounds. The higher energy driven into a bone the more likely it is to break. To help further the spongy cancellous bone absorbs day to day impact. Pop up to space with Elon Musk of Tesla fame and your bones won’t change, but spend a few months without gravity and bones can thin out and weaken. We need to walk and use our feet and leg bones to keep them healthy. We also need vitamin D for healthy bones but this means a healthy diet often called a mediterranean diet of oily fish, legumes and fruit. It might shock but evidence suggests that Vitamin D supplements will not prevent fractures while exercise and diet are vital. Vitamin D is essential to absorb calcium so any bowel complaints can affect this process. Osteoporosis is helped by vitamin D supplement where the main skeletal bones affected are vertebrae and pelvis rather than the foot. Sun light is important for healthy absorption of calcium. For the whole process to work we do need our liver and kidneys in good working order as this important in making vitamins absorb correctly. Black skin blocks light and so in the UK those with this ethnic type of skin can develop bone problems like rickets in the young.
Special note: Podiatrists are trained foot specialists and look for sudden fractures without a clear injury. Although rare, fractures can occur where bones have signs of cancer and these need to be ruled out by x-ray. Metatarsals are the commonest site. Cancers can spread (metastasise) from organs such as the lungs, bowels, kidney and liver.
Which bones are most at risk from fracture?
The longer the bone, the more prone to a crack or break. The second and fifth metatarsals bear the main brunt from injury. My wife sustained a 5th metatarsal fracture (see x-ray picture). There are two main types of fractures – open and closed. In addition, there are simple and complex fractures. Let’s put these into context.
Dangerous fractures
An open or closed fracture may well be complex because bones can tear soft tissues or, if not visible, may bleed inside and hide the damage. Falls in elderly are more dramatic because of loss of blood into the thigh, which has a big space to lose blood volume. The foot does not have the same concerns fortunately and such fractures with large blood loss are more obvious. Massive swelling after injury needs emergency attention. For the most part, most of these types of fractures are fixable, but the ankle is more open to long term damage as the leg bones connect to the talus. You can read more about ankles in fracture v sprains.
Road traffic accidents (RTA), occupational and industrial accidents are far more complex, and books have been written about all the variations. Grades of damage are listed for many fractures as type 1, type 2. There are several concerns. If the fracture is not easily put back into place, or if the fracture is badly displaced, then intervention is required to avoid long term damage, poor function and long term pain. Blood vessels and nerve damage must be rectified and repaired as early as possible. The RTA and the foot is a problem because the small bones and ends of the long bones are pushed together and split. In the midfoot this could cause long term disability and pain.
First, emergency services need to preserve life – airway, breathing and circulation. The foot will only be managed if life is stabilised and the limb is not impoverished due to a cut off blood supply. The less severe fractures described next may be cause problems depending upon where the damage arises and how much force is delivered through the foot.
Least dangerous fractures
Simple fractures usually mean no displacement of the overall shape as in complex open or complex closed fractures. However, let us move away from these types of fractures because this comes under moderate to significant trauma, which is the domain of the orthopaedic surgeon.
Stress fractures are usually the most common of all foot fractures. There is a difference between these and the previous type of fractures. First, a crack occurs, which may be partial or complete. In other words, the crack may not go all the way through. These need rest, some splinting if necessary, ice, and reduced weight-bearing. X-rays show a delay of 2-3 weeks so an x-ray looks normal to start with. Although scans are more sensitive earlier they are not 100% reliable if taken too soon. Scan imaging is more expensive than x-rays, and in the NHS (UK) such imaging has to be booked for an appointment, often delaying the diagnosis.
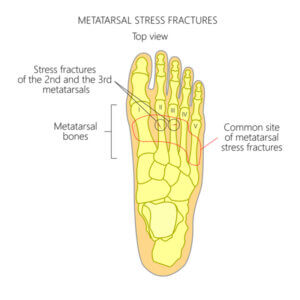
Stress fractures can arise around the neck of the metatarsals, often 2 and 3, but any can be involved. Stress fractures have also been called ‘march’ fractures as they used to occur in soldiers on parade because they stamp marched everywhere as a repetitive low grade force. As a result, the foot swells around the bone. The area is tender, and walking can be uncomfortable.
Displaced fractures can still be simple but are more than simple stress-induced and require more care. If two ends or pieces are reasonably aligned, even if a gap exists, this can be splinted in a walker boot (pictured below this article). We prefer not to use plaster of Paris or plastic casts because muscles can waste and bone thins (osteopenia) and swelling can pose a problem for shoes. If the fracture is in a number of fragments, this is more complex and may have to have open surgery. Surgery today uses plates, pins and screws. The diagram shows a displaced simple long spiral fracture of the fifth metatarsal shaft (the wife!). Treatment was walker shoe splinting, rest and gentle motion non-weight bearing for eight weeks. This took 12 weeks to settle, with some symptoms still occurring for a few months afterwards.

fifth metatarsal split shaft fracture female 74 after a fall.
The mechanics of these fractures occur when twisting movements arise together with the foot tipping over. The example was sustained when my wife fell backwards and twisted her foot going up some steps. The tendon on the outside of the foot adds to the problem and can pull back at its insertion. The foot then pivots around the position, and the weakest point yields and this is where the break arises. Although it is not possible to tell from an x-ray, her age was 74, where bone may have less strength than someone half this age. Post-menopausal conditions increase the risk of fractures in females. Age, or shall we call it physiological age associated with natural tissue ageing, makes fractures higher in the older patient. However, in a younger patient, the tendon may have pulled against the fifth metatarsal base instead of pulling the bone away. In this way, we see that different types of injury, age and medical health can set up in unequal proportions.
Falls, sudden twists, the constant pounding of the foot and dropping heavy objects can all create a fracture. Patients can sustain fractures in the small bones of the toes. It is usual to bind two toes together but avoid cutting off the blood flow by being too tight. In one case, I had to pin the fifth toe as it was taking too long to heal. Under local anaesthetic, a steel wire was inserted under x-ray guidance and left in place for three weeks. This fixed the problem, and the wire came out quickly without anaesthetic. The patient was a 45-year-old female who had reacted to the adhesive strapping.
Complex closed foot fractures
Chips and small avulsions
In many cases, small pieces are pulled away in foot bones and can be left, but these flakes of bone may require removal if symptoms persist. The ankle is a common place for flakes to chip off, especially around the outer ankle bones. In addition, the navicular and its bulbous inside, known as a tuberosity, can be pulled open. Because the tendon is crucial in the middle section of the foot, pain continues until management is undertaken. An avulsion is more severe because the tendon will keep pulling until the bone is stabilised, opening up the fracture site. (Navicular avulsion fracture).

Case courtesy of The Radswiki, Radiopaedia.org, rID: 11662. Note this is not an x-ray but an MRI scan using electricity & magnets rather than radiation.
Avascular fractures
This may sound more complex than it really is but avascular simply means without blood supply. If the fracture tears through the blood supply to the bone, the bone will lose density and fragment, squash so that it flattens or leads to poor healing and restoration. The most severe avulsion fracture occurs in the talus (ankle bone). Any collapse of the bone will have significant long term effects and should not be dismissed as a simple ankle sprain. The Jones fracture, affecting the fifth metatarsal base, is prone to poor healing because of loss of blood supply. Of all the bones, the fifth metatarsal is frequently injured in sports and of course my wife.
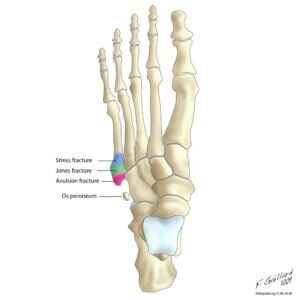

the Os perineum present left hand picture is an accessory bone and may not be present in all people.
In these diagrams, we can see different fracture types along the bone from the head to the base: stress fracture, Jones fracture, and avulsion fracture. Not all Jones’ fractures require surgical management, but the main objective is to stabilise the bone and casting with fixed casts may be necessary. I have, on occasion, fixed these fractures with surgery and the You Tube video (blue) shows the technique used today. Jones fracture fixation (C/O Sussex fracture clinic)

a tuberosity avulsion fracture of the 5th metatarsal can result in poor healing because the tendon continues to pull the fragment open
Taking action after a suspected injury
 To keep bones healthy we need a good diet of the right foods which includes calcium. We need to take exercise, have sufficient sunlight without sun stroke or skin burn, and we should keep our liver and kidneys working and check that we have healthy bowels with check ups as we age. And that’s all for healthy bones!
To keep bones healthy we need a good diet of the right foods which includes calcium. We need to take exercise, have sufficient sunlight without sun stroke or skin burn, and we should keep our liver and kidneys working and check that we have healthy bowels with check ups as we age. And that’s all for healthy bones!
This article discusses the type of fracture that does not require emergency management but should be seen within 5-10 days so that an x-ray can be undertaken after a professional clinical assessment. Fractures need assessment early if suspected. Use the NHS – 111 services if you are concerned rather than going to A&E. However, serious life-threatening injuries require 999 emergencies.
FRACTURE CLINICS is a common term used for an orthopaedic setting in the UK. Today, because of pressures, multi-disciplinary teams or MDTs have played a part in dealing with the less significant complications as part of triage within the NHS. Patients with more important concerns are passed onto orthopaedics.
Podiatric surgery is playing an ever more critical role in assisting the NHS to deliver parallel orthopaedic care given their surgical expertise. The role of the advanced practitioners in musculoskeletal services also includes podiatrists and is pivotal for playing an essential role in primary diagnosis. Emergency rooms and smaller hospitals exist in the USA and their approach to treatment is different and more intensive at an earlier stage than in the UK. Some of this difference is due to the funding of the two health services.
Does it matter which foot bone you break? Yes it does. I would go for the toe or central metatarsals but avoid the fifth metatarsal. Of course we should avoid fractures altogether but hopefully you now know a bit more than when you started reading.

- If you want to take your reading to another level then www. footeducation.com is a useful site. For more information on fractures and risk together with nutrition the are many sites but sometimes the medicine and science is more detailed.
- A useful quick reference from this US podiatrists about exercising after fractures can be found exercising after foot fractures.
You can also read more about pain in the foot on this site.
- Locating foot pain
- A Foot Condition called Freiberg’s
- Treating a complaint called Freiberg’s
- Ankle Fracture v Ankle Sprain
- Treating Simple Ankle Sprains
Thanks for reading ‘Does it matter which foot bone you break?’ by David R Tollafield

Published by Busypencilcase Communications Est. 2015
10th January 2022

Recent Comments