Medical challenges for podiatrists
Chilblains and their presenting features might well appear in the infamous list of conditions associated with podiatry such as IGTN, hard skin, corns and bunions. Podiatry is a medically based profession and has been for over 50 years when the original chiropody courses expanded with the older form of regulation. Recently Kriss challenged podiatrists to look at their own output. His article – What’s the point was a gauntlet challenge. Never has there been a more important time to align with the general practice of medicine. GP medical practice is withering in the face of recruitment challenges and targets. Our empathy is with medics. We are not against them but we have a duty as podiatrists to provide good foot health care. As primary health care specialists, where primary means first contact, we are the eyes and ears of traditional medicine. The degradation of the GP practice is something that we will be better able to analyse once the full extent of Covid-19 can be managed. I say managed rather than conquered as most feel we will be adapting rather than beating the virus by eradication.
 Since the start of this year, ConsultingFootPain (CFP) has produced some articles around the podiatry Facebook (FB) platforms where much debate about practice and patient concerns are posted. The resultant effect from a decent strand of respondents builds a picture and so CFP braids these loose strands together into a formal string that is a little more sustainable. CFP does not name any podiatry sites and believes that these and the respondents should remain anonymous as a rule.
Since the start of this year, ConsultingFootPain (CFP) has produced some articles around the podiatry Facebook (FB) platforms where much debate about practice and patient concerns are posted. The resultant effect from a decent strand of respondents builds a picture and so CFP braids these loose strands together into a formal string that is a little more sustainable. CFP does not name any podiatry sites and believes that these and the respondents should remain anonymous as a rule.
The list below emphasises some of the topics.
- Poor data collection exposed
- Pain after injections for nail surgery
- What’s this at the end of my toe?
- Should you write to the patient’s GP
- How should we write on Social Media
- The Ugh Factor – podiatry recruitment
Skin and podiatric dermatology
Of all the topics, skin is the constant. Personally, I don’t think podiatric surgeons (PS) are any more adept at giving advice than diabetic specialists (DS) are and so we defer to those with more knowledge and passion covering this condition. However, one important difference between general practice and those with PS and DS exposer is their ability to utilise medical facilities. Now I might appear as an evangelist here and if that is the case I can be happy but following on from Mr Kriss I feel we need to establish a more effective system of care. I came across the latest Medscape challenge and recommend all clinicians sign-up. It is a teaching resource around medicine and the best part is it is free!
If you are going to write about your case use the model in the Medscape challenge. Decide what tests you might wish to consider and arrange these so you can exclude other conditions. You have the knowledge to research a differential diagnosis which is achieved as a general rule by imaging, microbiology, clinical examination and blood tests. At the heart of any consultation lies the physical examination and workup. Before anyone becomes exorcised one should play to the accessible investigations but where these don’t exist, consider seeking specialist help. As a reader, I criticise narrow history taking and poor photos and you can read the occult frustrations from those trying to help. “She needs to see xyzzy…” Or, I cannot tell from the pictures. Dermatology requires good colour definition, feeling, as in touch for texture; the whole body needs to be visualised. Eyes, mouth, tongue, neck, thorax, hands are part of the examination.
And so we come to this article in camera. The chilblain. Skin problem or medical problem? In truth, this topic would never have galvanised me had three things not happened since March 2020.
- Medicine was challenged as a service
- Covid toe became a reality
- Podiatrists were inundated with dermatological shapes, colours and sizes.
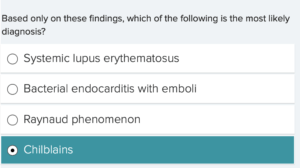
Tragedy? Far from it. It is a golden opportunity for podiatry to kick off from a different side of the swimming pool and thrive to help patients. With the help of Medscape Challenge, I have copied the two elements that stand out. I have put some headings in and attempted to explain a few medical nomenclatures. Read, digest and apply. Think outside the box.
Medscape Challenge
Background
A 43-year-old woman presents to the rheumatology clinic with a 1-month history of painful, discoloured toes. She first noted redness and itching at the tips of her toes about 2 months before presentation. The itching progressed to tenderness, followed by the formation of “sores” over the affected areas. She notes that the toes have been sensitive to cold, particularly when she leaves the house her feet, recent illnesses, or recent surgical interventions. The patient has never had similar symptoms in the past. She feels otherwise well and has not had any fever, joint pain, gastrointestinal symptoms, or weight changes. Her current medications include over-the-counter fish oil tablets and a daily multivitamin. She does not smoke tobacco and drinks three glasses of wine weekly.
Physical Examination and Workup
Upon physical examination, the patient’s oral temperature is 98.8°F (37.1°C). Her pulse has a regular rhythm, with a rate of 79 beats/min. Her blood pressure is 112/66 mm Hg. The head and neck examination, including auscultation of the carotid arteries and funduscopic visualization, is normal. Her lungs are clear to auscultation. The cardiac examination reveals normal S1 and S2 heart sounds, without murmurs, rubs, or gallops. Her abdomen is soft and non-tender, with normal active bowel sounds on auscultation. No abdominal masses or organomegaly are noted. Vascular examination reveals 2+ pulses at the axillary, brachial, radial, femoral, popliteal, dorsalis pedis, and posterior tibial regions, without bruits. The neurologic examination is nonfocal.
Skin examination
Dermatologic examination reveals non-blanching purpuric lesions overlying the pulp area of the right first, third, and fifth toes, as well as the left second and third toes, with superficial ulceration of the right third toe. The lesions are surrounded by poorly demarcated blanching erythema (Figures 1-3). The remainder of the dermatologic examination is normal, with normal upper-extremity nail-fold capillaroscopy.
Laboratory and tests
The laboratory findings, including a complete blood count and comprehensive metabolic panel, are normal. The prothrombin time and partial thromboplastin time are normal. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level, both inflammatory markers, are normal. Tests for antinuclear antibodies (ANA), antineutrophil cytoplasmic antibodies (ANCA), rheumatoid factor, lupus anticoagulant, anticardiolipin antibodies, antihistone antibodies, anticentromere antibodies, and cryoglobulins are all negative. Testing for acute and chronic viral hepatitis is negative. A lower-extremity arteriogram reveals patent vasculature with the normal-appearing flow.
Punch biopsy (histology)
A punch biopsy of the left second toe reveals both superficial and deep perivascular inflammatory infiltrate that is predominantly lymphocytic, superficial dermal haemorrhage, and a lichenoid tissue reaction/interface dermatitis (Figures 4-6). For those with more enquiry go to the site and take the challenge knowing you cannot fail to learn more about chilblains.
Medscape
Take the challenge
I will be honest I wanted to tick chilblains to start with but the histology and one of the tests wrong-footed me and I went for SLE instead. WRONG!! The fun bit about Medscape is that you pitch good educational information from experts against your knowledge without fear or fright. Never be frightened to get things wrong but it is best to make mistakes on paper and learn.

Take the challenge quiz here
What basic podiatry could do
Brief overview
ESR and C-reactive protein (CRP) are the most frequently used markers where you want to rule out inflammatory body responses to disease. Take an auricular temperature using a modern device first. The other blood tests are not routine and might be best undertaken by specialists. A Full blood count (FBC) is used with the inflammatory markers ESR and CRP and allows you to rule out significant iron and oxygen capacity alterations with RBC which can point to anaemias. Platelet populations are between 150,000 – 450,000. White blood cells show the range of neutrophils, lymphocytes, monocytes, basophils and eosinophils. Some suggest infection or leukaemia others show up as allergic reactions.
Blood pressure forms part of standard monitoring and is easy to perform with a regularly calibrated automatic cuff-sphygmomanometer. All patients should have their BP assessed as well as pulse. You can use Doppler for this and assess the heart rhythm at the same time. Tests for routine renal function starts with a urine dipstick test and a mid-stream urine sample valuable for picking up infections. All podiatrists would benefit from a haematology course or lecture and this is achieved by getting a local branch to invite a haematologist in to speak. Dermatoscope skills should be added to and much work is being carried out by Dr Ivan Bristow in this regard.
Podiatric surgeons attended haematology courses as part of fellowship from the 1980s onwards. All patients are routinely screened before general anaesthetic procedures and those over 50. Where infections arise, blood tests are used to evaluate the importance of systemic management by oral versus IV antibiotics. As clinicians gain more confidence they can expand their medical tests and assessments to best fit their specialty but GP podiatrists do need to ensure a good grounding upon which improved referral can be made. Remember you are not taking the place of the medical practitioner but facilitating faster pathways for the referral. Patients in the UK need to arrive at the right place at the right time without waiting. Private labs and NHS departments can offer access to many tests and will of course depend on the patient’s preferences and pocket.
If your practice does not offer quality diagnostic procedures everyone loses out.
Thanks for reading ‘Chilblains and presenting features’

Published by Busypencilcase Reflective Communications. Est. 2015

4th October 2021

Recent Comments