Chronicity and the Lateral Ankle Sprain
Reviewing the Ankle with Diagnosis in Mind
What this is about and what it is not about?
Chronicity and the lateral ankle sprain is written neither as a surgical article, nor one about fractures of the ankle which form part of acute trauma. The subject is limited to the lateral ankle sprain and tears. Medial ankle sprains arise but are generally rarer when compared to the lateral side of the ankle. When it comes to the anatomy involved in injuries, whether bone, joints, or soft tissue, the chronicity and lateral ankle sprain problems will vary. I have provided a quick reference to an excellent orthopaedic site covering key medial ankle problems offering valuable insights into additional ankle problems. This article is moderately easy to read [53] for the professional-clinical market. The reader can review my other ankle articles provided for lay readers and professionals.
THE MESSAGE
 when treating ankle problems:
when treating ankle problems:
Take a good history
Examine methodically
Treat conservatively
Treat early
Treat aggressively
Avoid surgery
Timeline
The aim behind this article is to ensure the reader understands that ankle sprains can lead to problems that either frequently reoccur or that symptoms fail to resolve over time. Timeline becomes a vital part of the understanding that poor results are associated with chronicity while acute ankle problems respond better where treatment is instigated early.
The hindfoot in perspective
Unlike the forefoot, the hindfoot has not been the focus of podiatrists compared to the forefoot. That said, the midfoot has a significant interest to the podiatrist and suffers from even more ignorance amongst general medical practitioners than any other part of foot anatomy. Put bluntly, ankle sprains occur frequently, but health care does not always deliver the best approach in the UK. Lack of timely care and action is often at the route of the problem. With the exception of trauma affecting function and life, trauma centres or A&E departments should not be used for first line approaches.
- Sprains are common especially when the ankle is unstable in plantar flexion and the body is moving at the same time beyond the joint’s stable position. Such straining or tearing ligaments and associated structures leads to wider problems.
- Damage does not just include the lateral ankle compartment alone.
- The secondary features of sprains and strained tissues can lead to longer term problems.
- Gait and mobility when affected compound chronic changes in the soft tissues
- Nerves that are damaged also compound the problem and are associated with scar tissue.
Three joints make up the ankle
The ankle is a big organ consisting of three main joints. The talo-crural joint, the subtalar joint and the talo-navicular joint all work together. It is important that we examine each separately and understanding their limits.
Each highlighted joint location takes you to a different article
The role of Musculo-Skeletal Services

With growing interest in MSK work in all health sectors, the involvement within the region known as the ankle has increased. Society’s interest in fun runs and marathons as well as extreme sports has accelerated over the last 50 years. The clinician will need to consider all three joints of the foot and ankle as well and undertake a full body and gait assessment. It is good practice to notate each aspect viewed and examined with both positive and negative comments for optimal record keeping. The areas break down into:
- Peri-ankle pain (soft tissue – ligaments and tendons)
- Bone & Joint pain (articular)
- Neurological & scar
APPROACH TO EXAMINATION & HISTORY
Joint examination must achieve three goals. Evaluate the range of movement, identify any limitations of movement and symptoms – R.D.Q.M
- Range & direction (refer to the links above ‘Three joints make up the ankle’)
- Quality involves limitations of joint
- Movement should be pain free and fluid
Range
The first port of call is to understand the anatomy of the hindfoot. Knowing what is where and what is normal? Of course when we talk about normal we must appreciate there are parameters affecting how much a joint moves. Evidence that at minimum of 10 degrees of dorsiflexion is required is based on EMG Studies (Yoon, 2013). Ideally we should find a total range of 60-70 degrees (Source: American Academy of Orthopedic Surgeons) for plantarflexion+dorsiflexion.
 Working out the chronicity
Working out the chronicity
We must consider pain but do ask about pain before the examination. You don’t want to hurt the patient needlessly. Go for the standard simple questions structure; WHEN-HOW-WHAT
- When did it happen? – timescale or TIMELINE
- How much pain /intensity? – VAS or visual analogue scale
- How long does it last? – is it short or long and sustained
- How far can you walk /stand?
- What makes it better? – rest, tablets, cold or heat
- What type of pain? – describe
- What makes it worse? – weight bearing versus rest
Be systematic
The old adage of LOOK-FEEL-MOVE is not new but remains important. Clearly an infected ankle should not be examined as aggressively as an ankle with normal dimensions. An oedematous ankle due to poor drainage or lymphatic pitting adds to the difficulties. We must do our best using all the anatomical markers we know and can see.
Quality, movement & impingement
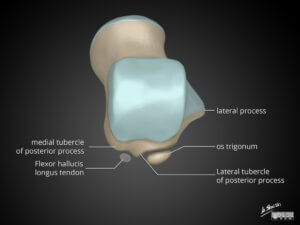 The Look-Feel-Move analogy must be conducted thoroughly. In the Kagar’s triangle we find the deeper calcaneal bursa between the tendo-achilles and calcaneus and the os trigonum proximal to the talus if present. Compressing tissues manually includes looking for distension using the ballottement technique for pouches of fluid moving around. Fluid within a normal bursa is difficult to palpate.
The Look-Feel-Move analogy must be conducted thoroughly. In the Kagar’s triangle we find the deeper calcaneal bursa between the tendo-achilles and calcaneus and the os trigonum proximal to the talus if present. Compressing tissues manually includes looking for distension using the ballottement technique for pouches of fluid moving around. Fluid within a normal bursa is difficult to palpate.
The ankle (TCJ) will move less in dorsiflexion than in plantarflexion. At the end of the range upwards (15-20o) and downward (45-55o) there should be an abrupt end to the range without pain or sponginess. When moving the ankle downwards the key concern is pain at the posterior of the TCJ where Steida’s process is an elongated part of the posterior tubercle of the talus. Impingement pain may signify injury, fracture and inflammation, common in dance, football and similar activities. In the upward dorsiflexed position, the impingement arises due to the tibia and talus having a bony bar (see below) or small fracture with or without a loose body. Both limitations may be painless as well as hurt
Investigations for lateral ankle sprains
- X-ray (See Ottawa rule)
- Ultrasound
- Magnetic Resonance Imaging (MRI)
- Computerised Tomography (CT)
- Nerve conduction studies
- Stress testing under anaesthetic
Investigations utilising imaging is important. X-rays for bone and joints, ultrasound for soft tissue, MRI and CT provide three dimensional views but as slices. CT can be ordered as a 3D picture. (See Ozkan)
OTTAWA RULE FOR ANKLE X-RAYS FOLLOWING INJURY
 We must include the Ottawa Ankle Rules in our discussion. Ian Stiell (1992) found too many x-rays were being taken for ankle problems attending the emergency centre. The rule applied universally attempts to reduce the cost and exposure of radiation. Principally it falls to the two malleoli and the fifth metatarsal with additional examination of the navicular. Also failure to walk for 4 steps. The rule does have limitations as found in a New Zealand study in 1994 when 21% of 350 ankle injuries showed fractures, one of the talus and one of the cuboid.
We must include the Ottawa Ankle Rules in our discussion. Ian Stiell (1992) found too many x-rays were being taken for ankle problems attending the emergency centre. The rule applied universally attempts to reduce the cost and exposure of radiation. Principally it falls to the two malleoli and the fifth metatarsal with additional examination of the navicular. Also failure to walk for 4 steps. The rule does have limitations as found in a New Zealand study in 1994 when 21% of 350 ankle injuries showed fractures, one of the talus and one of the cuboid.
SOFT TISSUE – LIGAMENTS AND TENDONS
what does it mean when the patients says she has weak ankles?
Injury and grading
These simple descriptions come from a UK source (BUPA). Sprained ankles can be graded to describe how bad the injury is:-
- Grade I. A mild sprain, which happens when you overstretch a ligament. You may have mild swelling, bruising and pain around your ankle, but you should be able to put some weight on your foot.
- Grade 2. A moderate sprain, which happens when you overstretch and partially tear a ligament. You may have quite a lot of swelling, bruising and pain around your ankle, and you may find it difficult to put weight on your foot.
- Grade 3. A severe sprain, which happens when you completely tear a ligament. The swelling, bruising and pain around your ankle are usually very bad. Your ankle may feel quite unstable (wobbly) and you won’t be able to put any weight on your foot without a lot of pain.

Ankle sprains produce bleeding, but much remains invisible
Examination
The grading system 1-3 will be used in this article but the clinical examination does not lead to a clear and accurate grading assessment. The basic ankle inspection should include looking at the talo-navicular joint at the point where the forefoot is moved on the hindfoot. Rotate the forefoot around the TNJ to check for pain and excessive movement. Move it up and down while stabilising the hindfoot. Although the talar surface is large and dome like, it is track bound by the navicular and deep medial ankle ligaments.
Next check the lateral side of the foot for the base of the fifth metatarsal. Pain over the tuberosity could be implicated in ankle inversion sprains and fracture. The ankle is weakest on the lateral side because the anatomy is less robust. The problem we face is when a patient says I have weak ankles. What does this mean and what should we do? In all probability patients mean they keep going over on the ankle. We must undertake a basic examination first and then consider a stress test if pain and walking is affected adversely.
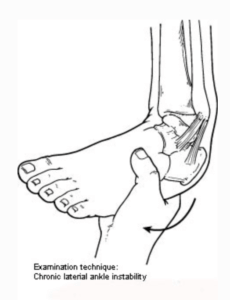
Lateral stress tests must be accompanied by rotational and antero-posterior (Drawer) shift tests. If the patient is suffering pain however or has oedema this is going to be difficult. Two choices exist. Carry out an ultrasound or MRI to check for ligament integrity, or undertake an examination under anaesthetic. For the purposes of conservative care, meaning non surgery, and non-injection therapy, a healthy suspicion may suffice that problems are not improving. However if the Ottawa Rules are used, then a baseline x-ray is essential.
Stress Testing
At least two views should be ordered AP, LATERAL & MEDIAL OBLIQUE, but ideally stressed. X-rays are notorious for being unreliable and using unprotected hands is not permitted under Health & Safety IRMER. This means clinical stress testing is unpredictable. ‘Guarding’ is the biggest problem with joint examination and you will see this in any joint after injury and in coalitions, described below. Tendons go into spasm to protect anatomy. To overcome guarding, anaesthesia can be used as a common peroneal block or general anaesthetic. The TELOS system has been available in North America for many years. Injury carries all the hallmarks of the inflammatory response which includes bleeding or haemarthrosis. Additionally the Telos system is nicely illustrated in Radiologykey.com and worthwhile reviewing.
Ankle sprain assessment is important because – the main components of the ankle lie behind their tendons and ligaments, each or together can be involved in damage. The antero-talo-fibular ligament is easily damaged (66%) and is involved in rotational forces. The calcaneo-fibula ligament additionally is involved in tears and ruptures (21%). The posterior talo-fibular ligament less so. The important superficial peroneal retinaculum however may be involved where this passes from the fibular malleolus to the calcaneus. Clinical examination alone can only hint approximately as to the exact tissue involved.
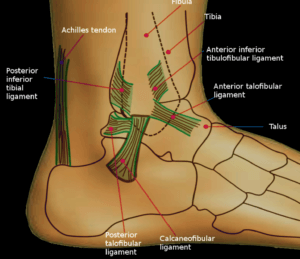
Chronicity and the lateral ankle sprain is associated with the anterior talofibular ligament and calcaneo fibular ligament in the main
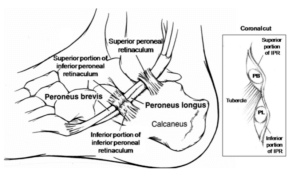
Peroneal tendons
Ligaments shown in the figure (in green) can be stretched with microtears and may recover with simple first aid. However continuous damage can create an incomplete tear. As with the knee and the anterior cruciate ligament, the ankle can be precariously positioned so that further damage and instability will continue. While we can focus on the ligaments, the peroneal tendons – peroneus longus and brevis are often both involved. The closeness of PB to the fibular groove means that trauma from inflammation can cause scaring and tethering. Tethering reduces the play in the tendon. Unable to overcome friction in its synovial sheath the tendon can tear. These tears may be complete or arise as split tears along the tendon length. The overlying superficial peroneal retinaculum can pull away from the periosteum in lateral ankle sprains. The PB can then subluxate causing a clicking with pain. Place a finger over these locations while moving the ankle through frontal and sagittal plane movement to identify the problems.
https://www.orthobullets.com/foot-and-ankle/7023/peroneal-tendon-tears-and-instability
Other forms of lateral ankle pain
Pain over the peroneal tubercle or trochlea should be ruled out. This lies on the lateral side of the calcaneus and divides the peroneus longus and peroneus brevis forming a pulley effect for tendon efficiency. The proximal band of the superficial flexor retinacular shares fibres with the tubercle. Hypertrophy may result from traction or may be enlarged as an anatomical feature. The peroneal tubercle therefore can be associated with pain and chronicity associated with lateral ankle pain. The reticular shown in the diagram are crude diagrammatic representations only.
The accessory ossicle os perineum can become irritated and is invested within the peroneus longus.
Bone & Joint Pain
Coalition

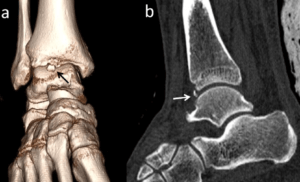
Case courtesy of Dr Brendon Friesen, Radiopaedia.org. From the case rID: 28726
Moving to the subtalar joint, often known as the talo-calcaneal joint with two major facets, the movement lies in favour of inversion by some 2-3 times that of eversion. And so 30-40 degrees of inversion against 15-20 degrees eversion may be apparent. If the inversion is limited, especially in children then suspect a coalition of the bony surfaces. In children these are asymptomatic and cartilage has yet to turn into bone. The problem occurs due to genetic mutation. Any limitations of the joint without pain may be associated with a bony block called a coalition.
Common coalitions
Coalition arises in the subtalar joint (talo-calcaneal – shown) and the calcaneo-navicular joint. Coalitions may occur without symptoms until an injury arises. At this point the patient may complain believing the problem to have been recent. When symptoms in the foot build, the shape may appear flat or adopts an everted position due to spasm. The CN joint coalition is easier to resolve than the ST joint coalition. Management is based on the severity of the problem and how it impacts on the ability to function at a socio-economic level.
Synovitis and joints
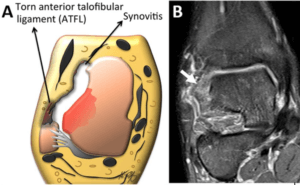 Chronicity leads to inflammatory joint changes. In particular, cartilage defects of lesions can arise in the lateral ankle or gutter. The lining of the joint hypertrophies adds to pain, swelling, limited movement and spasm reducing functionality. An MRI frontal plane image is shown against an illustrated impression. The white area represents synovitis.Cysts in the bone are identified as bone density changes on MRI, CT and sometime x-rays. Synovitis arises commonly in the long standing lateral ankle sprain and should be a prime suspect if conservative methods fail.
Chronicity leads to inflammatory joint changes. In particular, cartilage defects of lesions can arise in the lateral ankle or gutter. The lining of the joint hypertrophies adds to pain, swelling, limited movement and spasm reducing functionality. An MRI frontal plane image is shown against an illustrated impression. The white area represents synovitis.Cysts in the bone are identified as bone density changes on MRI, CT and sometime x-rays. Synovitis arises commonly in the long standing lateral ankle sprain and should be a prime suspect if conservative methods fail.
The other part of the ankle of note is the sinus tarsi or tunnel that exists between the talus and calcaneus. Within the ST the interosseous talo-calcaneal ligament exists. Sinus tarsi syndrome can arise with chronic pain related to injury although can arise through other causes including arthritides. But by far trauma plays the most common reason in ST syndrome.
Old fractures

Jones’ Fracture base of 5th metatarsal (X-ray MO and AP)
Fractures around the inferior articulation of the tibia-fibular includes syndesmotic strain between these ligaments associated with or without healed fractures. Closed fractures that have healed and have not been treated over time may be revealed. Chips and avulsions are more likely to cause problems because soft tissue tears the periosteal fibres and attachments (Sharpey’s fibres) are destroyed. Equally the bone anchorage itself may give cause loose bodies to arise. Pain at the site is enhanced when continuous traction persists and non-osseous healing. The fibula chip fracture is easily missed and not always picked up early on x-ray. This is probably because of poor or low calcium salts in the tissue which absorb radiation. Loose bodies in the lateral gutter or lateral trochlear surface add to the pain in ankles. Limited movement is certainly one indicator with pain. Cartilage softening and sub-chondral cysts form adding to inflammation and pain.
Two other bones that experience side effects from sprains include the base and tuberosity of the fifth metatarsal. The Jones’ fracture is different from an avulsion fracture and is chronic and heals poorly due to a poor blood supply and constant traction from peroneus brevis and lesser extent peroneus tertius. The other bone is the cuboid. Fractures, subluxation and synovitis between the base of the 4/5th metatarsals and cuboid can arise. Cuboid fractures may be more common in athletic sports than the regular less active population but walkers and anyone able to turn the ankle over is at risk. A small study by Jennings & Davies (2005) carries case histories for 7 patients aged between 15-36. Age however is no barrier to injury. The wary clinician should look to the obvious and then seek the hidden.
NEUROLOGICAL
Locating pain is not always easy in the ankle. Pain is often ‘referred’ and there are cases where a Morton’s Neuroma for example travels up to the ankle or shoots from ankle to toe. In this case examination of the key nerve routes will become important. These are shown by red arrows. On the LEFT side of the figure you can see the superficial peroneal nerve. On the RIGHT side the sural nerve can be viewed running behind the lateral fibula malleolus.
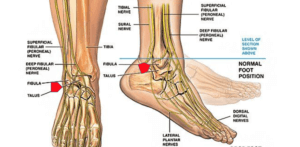 Tinel’s sign can identify the presence of nerve damage: chronic problems related to scar tissue contrasts with acute problems which are less track bound by scar tethering.
Tinel’s sign can identify the presence of nerve damage: chronic problems related to scar tissue contrasts with acute problems which are less track bound by scar tethering.
The sural nerve is a separate long nerve running behind the fibula and down the lateral foot. This should be percussed to rule out a positive Tinel’s sign. Neuromata affecting nerves can arise from injury because the sheath is involved with scar repair. More antero-laterally we see the lateral branch of the superficial peroneal nerve which runs close to the area where injury can arise. The ankle is also supplied by deep branches of the peroneal and tibial nerve. Pain associated with scar tissue from old haematomas can arise superficially and deep to the joint. Nitz et al (1985) reported on nerve injuries associated with sprains in 66 patients and compared grade II and III sprains. The peroneal nerve was injured more frequently than tibial nerve for grade II sprains but increased for grade III sprains. Tibial and peroneal damage must be included in the assessment as a cause of ankle instability. Return to walking was delayed for 5 weeks. This is a form of referred trauma causing the ankle weakness secondary the nerve lesion. The likely cause of injuries relates to nerve traction or a haematoma in the epineural sheath but can arise higher up the leg “at the bifurcation of the sciatic nerve into peroneal and posterior tibial branches. This report indicates that a consistently high percentage of patients with Grade III ankle sprains sustain a significant injury to both motor nerves in the leg and that rehabilitation time is markedly prolonged.”
Conclusion
A complex joint
The ankle is a large joint complex associated with larger and small gliding movements between leg and foot. The midfoot is just as likely associated with an ankle sprain as would be local ligaments. While acute sprains many settle without the need for intervention or long standing aid this is not the case for acute problems that become chronic due to improper recovery. Podiatrists alongside physiotherapists and chiropractors are first line advocates to help patients avoid long standing problems. The need for surgery should always be a last resort because this approach is not always successful. In part the reason for poor success is due to the range of pathology that arises outside simple ligament strain and its lack of understand by the patient and the inexperienced clinician.
Timeline factor
The decisions made to promote conservative care should be tempered by the the length of time an injury has been sustained versus the ongoing symptoms – this is the timeline factor. Returning symptoms due to a second injury should be treated more aggressively than the first. Diagnostic techniques such as x-rays in the first instance are important for chronic problems. Ultrasound, MRI and CT scans offering valuable insight and clarity because x-rays are not entirely reliable. The use of imaging is outside the remit of this article as is much of the treatment, but many links will take the reader to different options. Sobel (1992) provides a useful table covering the key headings associated with differential diagnosis.
![]() Highlighted blue text will take you directly to references within the body of this article and have not been replicated. Further reading is provided based on scientific articles that cover some aspects not covered within the talk. The volume of material on ankle sprains better known as ankle instability is extensive. The papers below represent scientific studies of interest to MSK podiatrists and physiotherapists.
Highlighted blue text will take you directly to references within the body of this article and have not been replicated. Further reading is provided based on scientific articles that cover some aspects not covered within the talk. The volume of material on ankle sprains better known as ankle instability is extensive. The papers below represent scientific studies of interest to MSK podiatrists and physiotherapists.
Further reading
Fuerst P, Gollhofer, A, Winning, M, Gehring, D. People with chronic ankle instability benefit from brace application in highly dynamic change of direction movements. JFAR. 2021;14:13 https://doi.org/10.1186/s13047-021-00452-0
Bavdek,R, Zdolšek,A, Strojnik,V and Dolenec, A. Muscle activity during different types of walking. JFAR. 2018 11:50 https://doi.org/10.1186/s13047-018-0291-0
Hiller, C, Refshauge, KM, Bundy, A, Herbert, RD. The Cumberland ankle instability tool: A report of validity and reliability testing. Arch Phys Med Rehab 2006;87:1235-41
Thanks for reading Chronicity and the Lateral Ankle Sprain by David R Tollafield

Published by Busypencilcase Reflective Communications for the Northern Ireland Branch of the College of Podiatry for a Webinar 9th March 2021

Recent Comments