Stretching. Does it work – a critical review of evidence?
Would it surprise you to know that plantar fasciitis confuses the medical profession? The reason is simple. The complexity of diagnosis and treatment options…
Accurate diagnosis & correct management
Diagnosis can be faulty and any treatment applied may be misjudged. Problems arise when the condition is assumed to be due to a heel spur; a piece jutting out of the bone, or that it will settle down with a tablet or capsule designed to deal with inflammation. It is misjudged because the length of time that the problem has festered means that there is no distinction between acute and chronic forms of heel pain.
Critical of doctors? Don’t be. They are generalists and feet don’t exactly take priority for most practitioners unless they themselves are runners. Furthermore, the literature is not exactly clear at times. Time has to be invested in diagnosis and treatment and that is when a foot specialist plays an important part.
 That first step in the morning…
That first step in the morning…
Ouch on first contacting the ground! Following that deep-seated tenderness around the heel, middle or inside front and in the arch of the foot, a needle-like sensation is often felt at its nuclear centre. The pain suddenly comes on and a specific association that caused the pain may not be easy to recall. The excruciating pain settles with a bit of walking because the nerves that relay pain ease after fluid built up within the heel pad clears. This is where the calf muscle pump is important. Activity removes fluid in the foot. If the fascial band is torn, then the relief effect may be less dramatic. Look at the picture of the fascial band below. Not what you expected maybe?
Treatment options are confusing
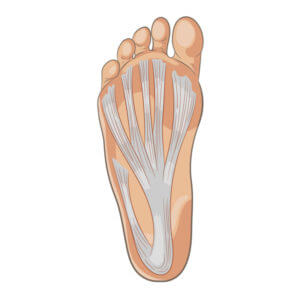
fascia band
Is it fasciitis? The problem with plantar (meaning sole of the foot) fasciitis is that pain affects the heel as much as the arch of the foot. If the pain shifts to the outside, well you probably are walking differently to relieve the heel discomfort. Not all heel pain is related to plantar fasciitis. There are other conditions that need to be ruled out. Fortunately, these are in the minority.
Today the options that patients face arise with growing interest from a range of clinical professionals. Pain and anti-inflammation medicines don’t deal with the cause of plantar fasciitis and therefore only aid with some of the discomfort. The best advice comes from education and understanding of the condition but this conservative approach seems to be limited in delivering benefits depending on how long the condition has existed.
Conservative approaches
Conservative methods such as stretching, taping and night splints should be used more, but as ever patients, and in particular runners want a quick fix. Clinicians are keen to find the best shortcut on behalf of their clients and often fear patients won’t listen to conservative methods.
Approaches for chronic plantar fasciitis
There are injections, the best known being steroids, a powerful anti-inflammatory drug. Another idea comes from spinning down components of the patient’s blood and injecting it back into the foot. Then there are electrical devices creating shock waves to stimulate the repair of the heel pad and the band known as the plantar fascia. And then we have surgery which mainly focuses on releasing the fascial band through a small hole in the skin. Surgery for the heel spur is no longer recommended and is rarely performed by foot surgeons.
How effective is exercise?
Evidence suggests yes, exercise is effective but combined, the effect of stretching exercises improves the results. The market is full of inventiveness as well as products that don’t make such a difference over home exercise strategies.The term exercise is used synonymously with stretching in this article.
In truth, there are more papers on heel pain than anyone could paraphrase in a short article, but concentrating on one aspect of treatment, stretching, does this really do any good?
Newswire (4 Nov. 2010) published an article based on the work of John Furia & others originally found in the Journal of Bone and Joint Surgery, a US orthopaedic paper. Of 102 patients 54 carried out stretching three times a day for eight weeks 65% were found to benefit as opposed to 29% who had received shock wave treatment.
A current paper in Foot and Ankle Orthopaedics
Lead clinical author (Kaiser, 2019) published and looked at 57 patients who carried out home stretches versus stretches under physiotherapy guidance after experiencing pain for three or more months. The follow-up period runs for 1 year as well as intervals of 3,6 months and 6 weeks. The overall conclusion was that home exercises were better and provided more sustainable improvement than relying on attending a clinical session.
The relevance here is that many treatment strategies can be conducted in the clinic under supervision. Better quality management appears to be in the hands of the individual who can devote far more time to stretching.
Effect on walking after treatment. Ioannis Agouris (2009) showed positive improvement in walking using a scientific method to analyse walking trends.
When should we start exercising? There is no absolute here, but the earlier you start an exercise to stretch both the Achilles tendon and fascial band the better. The main exercises are described next.
What exercise to use?
Exercises (Source:NICE (2015)
Achilles tendon and plantar fascia stretches are recommended using a long towel or Tubigrip around the toe end of the foot. Pull-on a thin towel with straight knees lifts the toes to the shin (dorsiflexion), and hold this position for 30 seconds. Repeat three times for each foot. Try and do this 2-3 times daily so building up slowly over weeks.
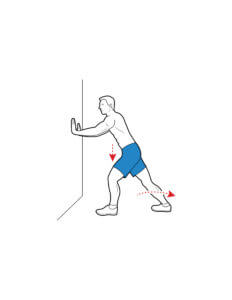
Wall stretch
Colin Hayes/Shutterstock.com
Wall push-up stretches for the Achilles tendon can be managed with the front knee bent and the back knee straight. The person should lean towards the wall until a tightening is felt in the calf of the back leg, and then ease off. Repeat ten times.The exercise above is repeated, but the back foot is brought forward a little so that the back knee is slightly bent. Repeat ten times. Repeat both sets of stretches at least twice a day. Stair stretches for the Achilles tendon and plantar fascia where both heels are off the end of the step, with the legs slightly apart. The heels are lowered, keeping the knees straight until a tightening is felt in the calf. The position is held for 20–60 seconds, and then the heels are raised back to neutral. Repeat the exercise six times, at least twice a day. Dynamic stretches can be used where the subject rolls the arch of their foot over a rolling pin, a sealed drink can, or a tennis ball works. Allow the foot and ankle to move in all directions as it rolls over the object. The exercise is continued for a few minutes or until there is some discomfort. Repeat the exercise at least twice a day.
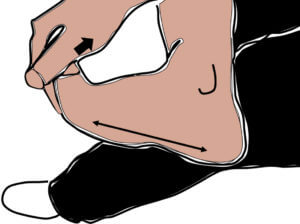
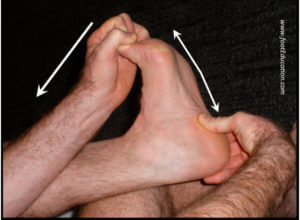
Stretches can be performed in the seated position. Cross your affected foot over the knee of your other leg. Grasp the toes of your painful foot and bring your ankle up and your toes up. Place your thumb along the plantar fascia and rub it to stretch it. The fascia should feel like a tight band along the bottom of your foot when stretched. Hold the stretch for 10 seconds.
Repeat it 10-20 times for each foot. Also be perform stretching initially in the morning, before getting out of bed and after any long periods of sitting. If there is a sharp pain in your heel when getting up, a stretch is best before standing or walking.
Is exercise likely to work alone?
More evidence for two different stretch methods
Engkananuwat (2018) recruited 50 participants for their article published in the US Foot and Ankle Society Journal. The paper focuses on both plantar fascia stretching and Achilles stretching. One group used Achilles stretching alone while the second group used both Achilles and fascial stretching. Achilles stretching intended to gain more upward ankle movement is a mainstay exercise that most people will be recommended.
The group of volunteers who stretched both their fascia and their Achilles tendons did better and showed they could cope with more pain pressure based on the evidence from an instrument measuring pressure as kilograms per square cm (Kg/cm2).
Night splints and stretching
Sallam (2016) looked at a larger group (75 patients) and combined stretching with a night splint. This meant stretch was sustained over the nighttime period rather than periodical stretching. The act of stretching and using a night splint showed more benefits than using a night splint alone or stretching alone. There was no clear idea in this paper how long people took to see the benefit. Improvement seems to show between 4-8 weeks.
How long should we exercise?
The act of stretching at all is better than nothing although no papers have looked at a pure control group in comparison (Landorf KB and Menz H, 2008). A control means one group has had no treatment while the other group has. The authors of this 2008 paper have not been taken up on their challenge it would appear 11 years later. Stretching should ideally be maintained for up to six months. All runners know to stretch before activity and so even if you don’t have plantar fasciitis building the stretch in would appear beneficial.
The stretch is repeated daily and held for several minutes with or without bursts of 30 seconds (repetitions). Bouncing on the calf is not advised but using a sustained stretch. Repeated several times a day helps.
Engkananuwat (2018) cited a protocol from another source, which probably was cited by someone else. That’s the problem with some papers. A stretching programme lasting for 5 days per week rather than 7 days with stretches performed at least 2 to 3 days per week by holding the stretch for 15 to 30 seconds and repeating 2 to 4 times. The total stretching time was suggested around 200 seconds per day, which was deemed sufficient for improving tissue flexibility. Clinicians are advised by The American Physical Therapy Association to use plantar fascia–specific and gastrocnemius/soleus stretching to provide short-term (1 week to 4 months) pain relief for individuals with heel pain/plantar fasciitis.
Heel pads may be used to increase the benefits of stretching. Although this varies from other guidelines, one is advised to use a programme that you feel works for you in terms of toleration and sustainability.
So is stretching your fascial band any good?
- An unqualified YES. But it depends on how chronic (+ 6 weeks) or acute (under 6 weeks), the problem has become.
- Combined stretching with night splints/socks is a firm favourite.
- Stretching both fascia and Achilles are important combinations.
- How long does stretching last? Well, it appears longer than 6 months with benefits from 4 weeks onwards.
 Further reading from ConsultingFootPain
Further reading from ConsultingFootPain
Protocols & Evidence
Professionally agreed strategies based on clinical evidence support the direction many clinicians use to help their patients. Protocols have been developed over years and from a number of sources.
[1] The American Physical Therapy Association has produced a serious protocol booklet revised in 2014. This is available on-line but the exercises are listed specifically. https://www.jospt.org/doi/full/10.2519/jospt.2014.0303
[2] NICE The British National Institute for Health and Care Excellence (link to recommendations) is awaiting an update in December 2019 but they produced advice about self-physiotherapy incorporating stretching exercises for the plantar fascia
[3[ Footeducation.com
https://footeducation.com/plantar-fasciitis/ provides information about stretches but leans more toward other modalities than self-help. Stretching for the calf and plantar (sole) stretch are shown.Source www.Footeducation.com
Thanks for reading ‘Plantar fasciitis and stretching’ by David R Tollafield
Sign-up for here my regular FREE newsfeed
Why not read Foot Health Myths Facts & Fables available from Amazon books
Published by Busypencilcase Communications Est. 2015 for ConsultingFootPain



What an AMAZING website from an accomplished clinician! Thank-you! I am near-crippled with what I’m self-diagnosing as PF (?!) and am finding your articles incredibly helpful.
Thanks again,
Rebecca.
Editor: Thank you Rebecca I am glad the article are of value. You can always share your experience with readers by writing about the journey. Please write to me at busypencilcasecfp@gmail.com if you are interested. David