Nurturing Female Pelvic Health
This month’s guest author is Carrie-Anne Martin, a UK-registered physiotherapist who has recognised the importance of post-natal pelvic floor problems. While this site emphasises foot health, musculoskeletal efficiency is altered in many ways. The pelvis is often forgotten as a component of pain, and clinicians, male or female, should be sensitive to the changes in the body after birth. As a professional and a mother, Carrie-Anne brings to light some of the preconceived ideas in her article ‘The Magic of the Pelvic Floor’ – packed with plenty of links to excellent sites and references. Editor
Who should read this article – professionals, lay people, and those affected by pelvic concerns following birth and incontinence?
§
Female pelvic health encompasses a wide range of crucial aspects that impact a woman’s well-being throughout her life. From the onset of periods during adolescence to the transformative journey of pregnancy and the challenges of menopause, women’s bodies undergo remarkable changes.
Pelvic health issues can have profound physical and emotional impacts on women’s lives. Making up 51% of the UK population, women spend a greater proportion of their lives in ill health compared to their counterparts. The symptoms associated with many of these health conditions, such as urinary leakage, pelvic pain, and sexual dysfunction, can lead to embarrassment, social isolation, and reduced self-esteem. Women may also experience limitations in daily activities and employment due to pelvic health problems. Addressing these issues is crucial to empower women, improve their overall well-being, and ensure their active participation in society. For the most part, we are led to believe that many of these issues are just ‘normal’ or par for the course of being a woman. Heavy periods, incontinence, painful sex, prolapse and suffering the symptoms of perimenopause are all part of being a woman, aren’t they?
Delays in referrals add to the emotional upset
As a Pelvic Health Physiotherapist I see the impact that pelvic health conditions have on the physical, emotional and social aspects of a person’s life. A staggering 1 in 3 females will suffer from incontinence at some point in their lifetime. Taking a minimum of 7 years to seek help and treatment, embarrassment silences them to manage with pads or leak-free underwear. These options are obviously great for the sanitary pad and underwear industry, which was valued at more than 10 billion US dollars back in 2020, but this means that the average woman spends £70 per month on incontinence products as a minimum. Whilst they provide temporary options for what are considered embarrassing and debilitating issues, they contribute to the normalisation of a condition that is not in fact, normal. Whilst it’s true that childbirth, menopause and ageing are all risk factors to incontinence, they don’t make it inevitable. Through a mixture of the right education and treatment, women can address these issues and compete on an even playing field. The unkept secret…….PELVIC FLOOR MUSCLES!
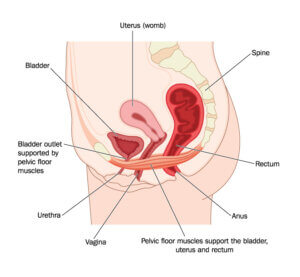
Pelvic floor muscles and their support of the uterus, bladder and rectum.
The Pelvic Floor
We all know that we have one, but 1 in 6 women have no idea where their pelvic floor is located or what its main functions are. Your pelvic floor muscles attach from the base of your spine to the front of your pelvis/pubic bone. They support your bladder, bowel and uterus and stop them from prolapsing, shut off the urethra and anal sphincters to prevent leakage of urine or faeces/wind, stabilise the joints in your pelvis and spine, and increase sexual pleasure.
Not all women with symptoms have weak pelvic floor muscles, but sometimes they need to learn to use their pelvic floor muscles in the right way and at the right time. Pelvic floor muscles should be kept strong and active, just like any other muscle in your body. It is well known that 40-50% of women will experience urinary incontinence in their 2nd and 3rd trimester of pregnancy, as well as in the immediate post-natal period. 10% of women will also experience anal incontinence (thepogp.co.uk). This can be extremely distressing and life-limiting, and many women believe that they are facing these symptoms for life. However, despite being extremely common, they are not normal, and women should now be offered routine pelvic floor assessments as part of their post-natal care (NICE 2021).
What are the symptoms of pelvic floor dysfunction?
- Stress Urinary Incontinence – Leakage of urine with activity, i.e. when you cough, sneeze, exercise or have sex.
- Urgency – A sudden need to go to the toilet, which may result in leakage if you don’t get there in time (urge incontinence)
- Frequency – Going to the toilet too often (more than every 2-4 hours)
- Nocturia – Getting up in the night to go to the toilet
- Bowel Incontinence – Leakage of wind or faeces after activity or because of urgency. This may also include difficulty getting clean after a bowel movement.
- Dyspareunia – pain during sex
- Pelvic Organ prolapse – A feeling of heaviness or something coming down in the vagina. Pain in the pelvic region or discomfort during sex. You may also be able to see or feel a plum-like bulge at the entrance to the vagina.
Risk Factors for Pelvic floor problems:
Pelvic Floor muscles behave like any other muscles in the body – they can be weak, over-stretched, torn or too tight. Just like how we hold tension in our shoulders and neck, we also transfer this into our pelvic floor muscles. Other causes of pelvic floor problems are:
- Pregnancy and childbirth – Pregnancy, in particular, lengthens and weakens the pelvic floor due to the weight of the growing uterus and the hormonal changes.
- Chronic Constipation – bearing down and straining causes weakening of the pelvic floor and can also worsen symptoms of prolapse. Sometimes difficulty emptying the bowels can be down to a tight and overactive pelvic floor.
- Chronic cough – Prolonged bouts of coughing can put extra strain on the pelvic floor, causing weakening of the muscles and stress incontinence.
- Menopause – Decreases in female hormones affect how well-supported the pelvic organs are and how well the pelvic floor muscles work
- Smoking – this can cause a chronic constant cough
- Heavy or repeated lifting – poor technique or excessive loads can increase the intra-abdominal pressure, which puts extra strain on and weakens the pelvic floor
- High-impact activity – Returning to high-impact sport too soon after having a baby or increasing your workouts too quickly and vigorously can overload the pelvic floor.
- Being overweight – increases the strain on the pelvic floor muscles.
Preventative measures:
- Doing regular pelvic floor exercises (particularly throughout pregnancy and just after having a baby)
- Maintaining a healthy weight
- Avoiding constipation
- Adopting the right technique when lifting and exercising and building up gradually.
Pelvic Floor Exercises:
Pelvic floor muscle exercises (sometimes called Kegels) should include long, held squeezes as well as short, quick squeezes; ensuring that you let the muscle ‘go’ or ‘relax’ after each squeeze.
You can locate these muscles by imagining that you need a wee and to pass wind, and you’re trying to stop both of these things from happening. The feeling is one of a squeeze and lift in the vagina and around the anus. Holding your breath or squeezing your thighs and/or buttocks is discouraged.
You should work the muscles until they tire and do the exercises regularly to help the muscles become stronger and more effective. Aim to be able to do ten long squeezes, holding each squeeze for 10 seconds, followed by 10 short squeezes. You should do your pelvic floor muscle exercises at least 3 times each day. You may find it easier to start your programme when you are sitting or lying down. Build up your exercise routine gradually over the weeks and months. You should notice an improvement in 3 – 5 months and then keep practising your pelvic floor muscle exercises once a day to maintain the improvement. As your muscles improve, aim to do your exercises in other positions, such as standing up. Eventually, you can practise using these muscles whilst doing activities such as walking and bending.
The National Institute for Healthcare and Excellence now recommends that Healthcare professionals should:
- Encourage women of all ages to do pelvic floor muscle training and explain that it helps to prevent symptoms of pelvic floor dysfunction.
- Encourage women to continue pelvic floor muscle training throughout their life because long-term training continues to help prevent symptoms.
- Encourage women who are pregnant or who have recently given birth to do pelvic floor muscle training, and explain that it helps prevent symptoms of pelvic floor dysfunction.
- Consider a 3-month program of supervised pelvic floor exercises, from 20 weeks of pregnancy, During postnatal care where there has been birth trauma, and for the treatment of urinary incontinence or prolapse
If you have pelvic floor issues or you’re unsure whether you’re doing these exercises correctly, a Pelvic Health Physiotherapist (POGP) can help. You can find your nearest one through the Squeezy app directory or the POGP website. Don’t suffer in silence!
Online Resources
- https://www.yourpelvicfloor.org/
- https://www.wellbeingofwomen.org.uk/
- https://thepogp.co.uk/
- https://squeezyapp.com
- https://masic.org.uk/
- The Well HQ : The Well HQ (thewell-hq.com)
- WHC factsheets and other helpful resources – Women’s Health Concern (womens-health-concern.org
Getting help from Carrie-Anne
image
Nottingham-based Carrie-Anne Martin is a Specialist Pelvic Health Physiotherapist and works Rushcliffe Physiotherapy and Sports Injury Clinic, The Spire Hospital and The Park Hospital, as well as The Menopause Consortium.
She is happy to be contacted:
- Email: carriemartin.physio@gmail.com
- Instagram: _pelvic_health_physio
- Facebook: Carrie Martin
![]()
- GOV.UK. (n.d.). Women’s Health Strategy for England. [online] Available at: https://www.gov.uk/government/publications/womens-health-strategy-for-england/womens-health-strategy-for-england [Accessed 8 Aug. 2022].
- thepogp.co.uk. (n.d.). Bladder and Bowel Incontinence. [online] Available at: https://thepogp.co.uk/patient_information/womens_health/bladder_and_bowel_incontinence.aspx.
- www.nice.org.uk. (n.d.). Recommendations | Pelvic floor dysfunction: prevention and non-surgical management | Guidance | NICE. [online] Available at: https://www.nice.org.uk/guidance/ng210/chapter/Recommendations.
- Meers, D. (2022). A case study project to establish effective delivery of physiotherapy-led pelvic health education among women during the childbearing year. Physiotherapy, 114, pp.e61–e62. doi:https://doi.org/10.1016/j.physio.2021.12.317.


Recent Comments