Skin Problems
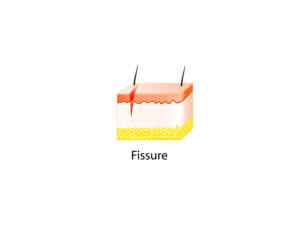
When it comes to skin and the foot, we will be familiar with corns and calluses. For many, hard skin relates to pressure and wear and tear and is something, we can manage with a bit of pummicing or reduction with a proprietary skin reducer. Thick skin is often called hyperkeratosis, which means increased keratin. Keratin is the top layer of skin and has no cellular nuclei. Packed tightly, the skin can act as a barrier preventing infection and allow normal comfortable walking. If the skin cracks or splits, the gap creates a fissure. The small blood vessels and nerves are exposed once this descends to the layers between the keratin and the softer tissue called the dermis. If this arises, the foot becomes sore and is at risk of bleeding and infection. Using resources and forming a quick guide, hopefully, the reader will find this article helpful.
 A QUICK GUIDE
A QUICK GUIDE
‘ConsultingFootPain’ provides readers with reliable information from trusted sources. I have listed the questions English speakers might consider helpful without a sales pitch.
- Why do fissures arise in feet?
- Can we prevent them from occurring?
- What current advice is available?
- Why consult a foot practitioner or podiatrist
Finding Quality information
Healthline provides an excellent article by Annette McDermott (March 2019). The second source is Medical News Today which similarly covers the same topic by Rachel Nall (May 2021) (see the origin of these sources at the end of this article). There is little point in copying or replicating these two excellent, detailed articles. However, let’s look at the content, summarise and allow the reader to dig further as required.
(1) Why Do Fissures (skin cracks) Arise?
There are medical reasons and causes relating to the mechanics of skin. Skin sits on a bed of elastic tissue. Because it contains a high percentage of water held between the cells, it can absorb a variety of pressures and forces associated with daily walking or contained within footwear. To make skin stronger, the protein called collagen braces the deeper tissue. You may wonder then why the top layer splits. Most TV ads talk about hydration and then cover mind-boggling chemicals you must have in your creams and lotions. Assuming that you have no hormone imbalance and no genetic problems with the skin that alters the skin’s strength, most cracks are occupational or related to weather and footwear. There are three main areas for skin cracks.
The toe
The skin is thicker on the pulp of the toe, and although any toe may be affected, the inside edge tends to carry significant stress. The skin moves as we push off when walking, setting up tension or tensile forces. Skin that is dry or has poor elasticity and strength can split at this point.

The skin on the sole of the big toe is very dry, making it cracked. This makes dirt accumulate, making the skin open to infection.
The Ball of the Foot
The sole surface is called the ball of the foot and also experiences considerable pressure when walking or running, and the foot twists across this surface. In a similar way, the skin, if dry, will respond to small tears, although not as badly as the toe or heel. In the cases of the ball of the foot, people who suffer the most tend not to wear shoes, or those worn are in poor repair, or they have thickened skin and might be malnourished. The illustrated picture (James Heilman, MD/Wikimedia) below is associated with fungal infection (Source:Medical News Today).

The condition shown is severe and requires professional help. As far as actions are concerned, I will cover this in the discussion under point (3).
The Heel
Early signs should be noted and action taken. Skin responds well to creams at this point but must be applied regularly, as in daily use. The top picture shows the skin is dry, with numerous streaks of skin developing in the top layer of the skin. The skin may be sore at this point. The lower picture shows full-thickness cracks, likely to be painful and bleed.

Early signs of cracked heels.

Advanced cracked skin leads to fissures.
Skin fissures can affect all genders, but footwear design can be an influencing factor. The shoe that causes the most problems is the mule or a shoe design that has no heel counter or strap. This allows the heel to slip but can cause the skin to bulge over the edge of the heel. This extra tissue distortion causes skin the thicken and then crack. Cold and damp weather can affect the skin as much as overuse of these shoe designs.

Women’s sandals. The skin of the heel overhangs the back of the shoe, causing tensile forces to act across the skin.
(2) Can we prevent skin cracks?
Some skin types are more prone. Most clinical pictures feature white skin, but darker skin is equally affected in the wrong conditions. The first important consideration is how did the cracks appear. Were shoes responsible or a type of activity? Did this happen during one period, perhaps? Next, ask yourself if you are suffering from or have a diagnosis of any skin condition, suffer from a medical problem or feel you have a vitamin or mineral deficiency. Seek medical assistance if you have other symptoms from urinary infections, blurry eyes, feel lethargic, or fail to heal after cuts. Check shoes for damage and design and alternate footwear to prevent fungal infections or build-up of sweat.
Basic foot care
Keep your skin moist with a proprietary skin product. The problem with the marketplace is that there are hundreds of products called emollients, and spending a fortune on products with ceramides and hyaluronic acids is unnecessary. The UK NHS site is useful for starting or visiting your pharmacist. In most cases, avoid fragrant creams and ointments. Creams for daytime use and ointments for nighttime. if the skin itches, you require something soothing. One of the preferred products chosen by podiatrists is Flexitol heel balm.

The product contains urea and helps with dehydration. As with all products, one size does not fit all. Some experimentation is required.
(3) Current Advice and Self-Management
Simple Splits
If you have the simpler appearing cracks, this is managed by the immediate emollient application. Reduce the skin hardness with any safe callus reducer from pumice, abrasive sponges, diamond deb files and electric roller abrasives. Apply emollients at night and under bed socks if likely to stain the sheets.
Avoid footwear that increases cracking. Apply a flexible collodion or skin glue. Germolene (Bayer) liquid plaster can be built up across the fissure in layers, allowing each application to dry to a film that covers the skin and fills in the crack. Healing occurs under the flexible film, and soreness disappears quickly after an initial stinging effect. The film is useful for cracks reaching the sensitive nerve endings. If the problem returns, repeat each stage.
- reduce hard skin
- apply emollient if the skin crack is not too deep
- for deeper cracks use plastic film
- Avoid the type of footwear if the cause
Moderate to Severe cracking
This type of problem may not be completely resolved by self-treatment. The frequency of build-up of the callus and the depth of the splits should direct you to find assistance. Once you can manage the skin, after professional guidance from a podiatrist or foot health practitioner (UK), you can treat the skin with simple splits.
- The clinician will assess the cause and provide advice.
- The skin will be reduced to ridges softened using scalpels and disks to reduce the bulk safely. Once the skin is thinner, the forces will reduce to the continuous strain, and creams and lotions will be better able to penetrate the skin.
- Sometimes, the skin must be wrapped in a plastic film overnight to improve emollient penetration.
- Any wound can be treated to minimise infection. Use of emollient dressings can be applied.
- Special heel cups may reduce the acting forces causing splits around the heel after footwear advice is offered.
- Once the skin is under control regular reduction with an abrasive roller will keep the thickness down.
(4) Why consider a specialist
Once you have been assessed and advice offered, the heel or other parts of the foot can be self-managed using the tips and advice. As with the two key articles referred to, it is important to ensure that there are no medical causes that should be attended to, as well as the skin. The worst type of fissures are very difficult to self-manage safely, and this should be of paramount importance. Debulking skin is a skilled task, and the only people who can offer such a service are podiatrists in severe cases. Trained with many hours of clinical scalpel management, they can help efficiently and safely.

Battery abrasive roller is available from outlets and is a safe method to reduce skin thickness.
If the origin of the skin problem has an inflammatory basis, then different skin products may be advised. While there is no guarantee the skin can ever be resolved completely, the recurrence of fissures can be managed.
RECOMMENDED SOURCES USED IN THIS ARTICLE
Healthline Media, Inc. is an American website and provider of health information headquartered in San Francisco, California. It was founded in 1999, relaunched in 2006, and established as a standalone entity in January 2016.
Medical News Today is a web-based outlet for medical information and news targeted at the general public and physicians. All posted content is available online, and the earliest available article dates from May 2003. The website was founded in 2003 by Alastair Hazell and Christian Nordqvist. Based in Brighton, UK
Thank you for reading this article, ‘Skin Cracks & Fissures on Feet’, written for ConsultingFootPain by David Tollafield and published by Busypencilcase Communications.
David is a former podiatrist, clinical teacher and author, as well as a Fellow of the Royal College of Podiatry. You can read more ‘about’ him on this site.

Busypencilcase Communications Est. 2015


Recent Comments