Academic assessment of the corn treatments – Part 2
Aim of treatment
The NHS site covers corns and calluses and offers safe but pedestrian advice. The pharmacist does not have training in podiatric medicine and provides a commercial enterprise offering skin treatments and pads, which can assist some but are not appropriate for all. Assuming the corn has not been infected, you can still try the remedies offered on the NHS site.
Today we know more about the humble corn than we have done in the past, but for many patients, sharp dissection on a cyclical basis is a quick fix, even if it is not permanent. Unlike a callus, however, your approach must be considered more cautiously. Part 1 covers some of the reasons why everyone needs to be aware that a corn may appear simple but may not be. Most patients would be happy to have the corn removed permanently. Others accept routine reduction keeps the foot comfortable. If a lesion is relatively new, the chances of responding are encouraging. Scalpel treatment alone is disappointing. CFP looks at some of the evidence behind concerns about chemical treatment and briefly looks at surgery.
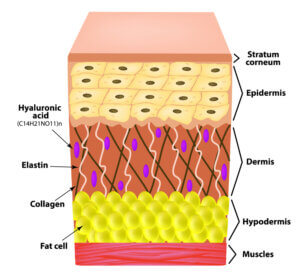
The fat or hypodermis is shown together with the illustrative arrangement of collagen and elastin, which offers flexibility to the skin.
If the corn does not respond over a period of several months, then there are diagnostic techniques, such as ultrasound, that can rule out problems within the hypodermis (fat) layer. Some podiatrists have reported complete resolution of corns, but there is no assurance from longer standing lesions and infection may have occurred.
Injectable and chemical treatment
Salicylic acid
This product can come in several forms, from liquid to pastes. Available over the counter, each product comes with instructions. Salicylic acid (SA) is usually only used on the skin of feet and hands. The concentration of SA available to the public is usually under 20%, but even this can cause damage without careful preparation. Failure of the corn to be managed lies in the lack of correct preparation or incorrect product use. The chemical softens the corn and, in some cases, will allow the core to disappear. Most podiatrists do not recommend self-treatment as there are risks even if the public does find the SA medication helpful.
Farndon and co-workers conducted a controlled study in 2014 on 202 participants. The study was carefully carried out, and patients were followed up at three and twelve months. Pain resolved in many cases and showed better results than scalpel reduction alone. Their statement contains two important facts. The use of SA prolonged the corn’s reoccurrence, and secondly, SA (40%) was under podiatry supervision, which was why many in the study did so well.
Podophyllin
Akdemir used a mix of SA (30%), cantharidin (1%) and podophyllin (5%) as Canthacur-PS. As before, SA is often used in wart treatment on the surface skin of feet and hands. Cantharidin is a toxic ingredient secreted from a beetle, and podophyllin comes from the roots of the mayapple plant. The product used by Akdemir was used as an alternative treatment for ‘callus’. Again the research method included professional debridement with scalpels. The skin blistered, which had a risk of infection and was covered. Most patients (79%) had one treatment – 72 patients. Some patients in the study had treatment for their hands, while 90% were treated for foot callus/corns. An antibiotic dressing was used following treatment and covering the wound for 7 days. Follow-up was one year, and only one occurrence was recorded. This type of management would require professional supervision.
Bleomycin
Lee (2014) followed the same protocol used in Farndon’s research on SA but used an antibiotic, usually indicated for cancer management, for corns on the sole of the foot. The drug has antitumoral properties and is antibacterial and antiviral.
Fifty male patients selected from military forces had a total of 64 corns. One group was treated with bleomycin and debridement, and the others with debridement. In this case, bleomycin was injected with an anaesthetic. The treatment was 37% effective, but in some, the corn failed to clear, but the pain was reduced. When compared to mechanical debridement, only 10% improved. Partial improvement was recorded at 43%, so in real terms, 80% benefitted from this type of treatment. However, on average, 4.3 treatments were required, and over 60% needed paracetamol for post-injection discomfort. The follow-up period was around 3 months.
Silicone Injection
Tollafield (2001) looked at thirty-one subjects with corns and used 350-centistroke polydimethicone or saline over a 6 to 9-month period. The subjects were equally divided between male and female. The concept of silicone acts as a filler to compensate for the loss of the hypodermis (see diagram). The idea for feet originated from Sol Balkin.
Two randomly divided groups received silicone (16) and sterile saline (15). Essential histopathology was randomly undertaken on 11 subjects. While granulomatous reactions were only positively identified in one case, the author identified a problem with two other participants at 15 years. This study found no evidence to show that small quantities of medically prepared liquid silicone caused adverse reactions, although two cases were more sensitive after silicone injection. The ‘silicone experiment’ was published in 2021by the author, 20 years after conducting the original work with Balkin (Tollafield, 2021).
The use of chemicals has been well known and applied for several centuries and has included caustics such as silver nitrate. Older podiatry texts colourfully include remedies from times past (Le Rossignol, 1971). Many are unavailable today, and some are not considered effective.
Other over-the-counter remedies
Pharmacies sell corn pads as rings of felt to protect the area. These should be used for limited periods only as the skin can be easily damaged if these pads become wet or the skin is poor or sensitive.
Gel plasters do not contain SA but soften the corn by adding hydration to the skin. Currently, salicylic acid is the only viable treatment sold for use by the public.
Surgery
Surgery to the forefoot is the last stage consideration but has a place for those corns, often known as intractable (plantar) keratoma, which causes pain and disability. Punch biopsy analysis (Güngör, 2014), full excision (Lopez & Kilmartin, 2016) and plastic skin coverage (Saipoor & Maher, 2018), electrodesiccation (Bevans 2010) and microwave (Case Reports Bristow, 2020) have been considered interventions. Some corns can affect tendons, and the author has published several articles on corns and calluses.
While microwave and freezing (cryotherapy) provide lesser surgical techniques, their success and mode of action are still not wholly explained more than replacing fat with a full-thickness skin flap.
The punch around a corn although successful in some hands does not always work, and it was considered a question of whether enough skin had been removed in the lesions that failed. However, when Lopez reports recurrence, the wider excision again leads to the question of why such lesions fail and return to the effects of smoking.
Hopefully, this article, together with Part 1, provides insight into why corns are difficult to manage and that, despite all our knowledge, a conclusive treatment still eludes us in the 21st century. CFP considers in almost all cases, patients should consult a podiatrist. Mechanical means of removing a corn by superficial enucleation is fraught with disappointment unless the pressure can be relieved with insoles or orthoses.
![]()
- AKDEMIR, O., BILKAY, U., TIFTIKCIOGLU, Y.O., OZEK, C., YAN, H., ZHANG, F. and AKIN, Y. (2011), New alternative in treatment of callus. The Journal of Dermatology, 38: 146-150. https://doi-org.libaccess.hud.ac.uk/10.1111/j.1346-8138.2010.00978.x
- Bevans, J.S. & Bosson, G. 2010, “A comparison of electrosurgery and sharp debridement in the treatment of chronic neurovascular, neurofibrous and hard corns. A pragmatic randomised controlled trial”, Foot (Edinburgh, Scotland), vol. 20, no. 1, pp. 12-17.
- Bristow, I.R. & Webb, C.J. 2020, “Successful Treatment of Hard Corns in Two Patients Using Microwave Energy”, Case reports in dermatology, vol. 12, no. 3, pp. 213-218.
- Farage, Miranda et al. from Cutaneous and ocular toxicology. Structural Characteristics of the Aging Skin: A Review. DO – 10.1080/15569520701622951
- Farndon LJ, Vernon W, Walters SJ, Dixon S, Bradburn M, Concannon M, Potter J. The effectiveness of salicylic acid plasters compared with ‘usual’ scalpel debridement of corns: a randomised controlled trial. J Foot Ankle Res. 2013 Sep 24;6(1):40. doi: 10.1186/1757-1146-6-40. PMID: 24063387; PMCID: PMC3856524.
- Güngör, S., Bahçetepe, N. & Topal, I. 2014, “Removal of corns by punch incision: a retrospective analysis of 15 patients”, Indian journal of dermatology, venereology, and leprology, vol. 80, no. 1, pp. 41-43.
- Lee, W.J., Lee, S.M., Won, C.H., Chang, S.E., Lee, M.W., Choi, J.H. and Moon, K.C. (2014), Efficacy of intralesional bleomycin for the treatment of plantar hard corns. Int J Dermatol, 53: e572-e577. https://doi-org.libaccess.hud.ac.uk/10.1111/ijd.12586
- Lopez, FM Kilmartin TE Corn Cutting in the 21st Century. Podiatry Now. October. 2016
- Le Rossignol.J, N, Holliday, CB A Pharmacopoeia for Chiropodists. Faber & Faber Ltd. 1971
- Saipoor, A., Maher, A. & Hogg, L. 2018, “A retrospective audit of lesion excision and rotation skin flap for the treatment of intractable plantar keratosis”, Foot (Edinburgh, Scotland), vol. 34, pp. 23-27.
- Injectable Percutaneous Polydimethicone in the Treatment of Pedal Keratomas: A Single-Blind Randomized Trial. Tollafield DR, Holdcroft DJ, Singh R, Haque MS. Foot and Ankle Surgery. 2001. 40(5):295-301
- Tollafield, David R Foot Health Myths, Facts & Fables. Podiatry Reflections. Published by Busypencilcase Communications, 2020. The Silicone Experiment. pp.204-206 (Available from Amazon Books)
- Tollafield DR Musings about corns and callus. May 2022. ConsultingFootPain
- Tollafield DR Obstinate Corns over Tendons October 2022. ConsultingFootPain
- Tollafield DR Hard skin on our Feet. November 2022. ConsultingFootPain
Thanks for reading ‘Treating Corns on Feet – Part 2’ by David R Tollafield
Published by Busypencilcase Communications. Est. 2015

David is the author-editor of ConsultingFootPain (CFP) and a former podiatric surgeon. Articles are published each month on this site. Sign up for his newsfeed

Recent Comments