Understanding what happens to the toe
Let’s talk about the reason big toe joints hurt to understand what is happening and why you might need help. Of course, we can always make the discussion complex, but that is not the intention. We just need to understand the workings of joint pain. ‘Hallux’ is Latin for big toe. You can get 16 points in scrabble for this word. ‘Rigidus’ obviously means stiff but ‘valgus’ means a deformity that bends out. If you want to true definition of valgus it starts to become complicated as podiatrists combine words like abducto-valgus to show two directions of deformity. The toe can be deformed, stiff or both deformed and stiff.

The right foot shows hallux valgus. Note it is twisted as the nail faces toward the painted finger nail. The bump is often known as the bunion
Arthritis
I confess I am not keen on the word arthritis as it conjures up a disease of the worst kind. So let us use the phrase ‘arthrosis’ because the term means a condition associated with deterioration of any joint, not just the big toe. Severe forms of arthrosis come under a wonderful term – the arthritides (arth-rit-eedees), which sounds like a Jason and the Argonauts crew member in Greek mythology. Rheumatoid arthritis and gout are two such conditions which are highly destructive. Already you can see Latin and Greek in our language. Medical people love to make everything sound complicated; a bit of old language helps!
Clinicians
Many seek help from the doctor (GP in the UK, internist or family practitioners in the USA), podiatrist or orthopaedist (orthopedist – US spelling). In both the US and UK podiatric surgeons and orthopaedic surgeon will manage big toe problems if surgery is required.
Examination

hammer toe
The clinician will start off and see how much movement you have and determine if there is pain in the joint. With hallux valgus (HV), the bump on the side hurts in many cases. In other words, the skin is damaged in some way. In addition, there may be a swelling (ganglion). The bump part is often called the bunion. With HV, the foot widens, and this causes other problems such as hammer toes, dislocation of toes and neuroma (Morton’s).
Even if the joint does not hurt or is damaged, the secondary features cause the problem.
When you try to bend the toe, it hurts. This will not just affect sports but can impact daily life. The big toe can move through 90 degrees, even when standing sits extended at 20 degrees. The joint should be free of pain when pushed, and if squeezed, the joint should neither be swollen nor tender.
Let’s talk a bit about anatomy
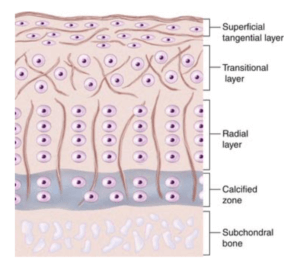
A millimetre is the smallest measurement on a school ruler. The cartilage covering the ends of the bone making up the big toe joint is less than a mm, which is thinner 1/16th of an inch if you use imperial measurement. That is pretty thin. The hip joint cartilage is between 2-3mm.
Cartilage contains water, special cartilage cells (chondrocytes), and a spidery framework called collagen, a protein and some sugar-protein molecules that push from each other maintaining tension. Those molecules (proteoglycans) have chondroitin and hyaluronic acid. Chondroitin is promoted as glucosamine in tablet form in health food shops. The molecules we know from school are just chemicals bonded together as short or long chains. The PGs (proteoglycans) are essential for maintaining healthy cartilage. Unfortunately, as we age, the cartilage becomes brittle as the substance of collagen, chondrocytes and PGs reduce.
Exercise helps keep joint healthy
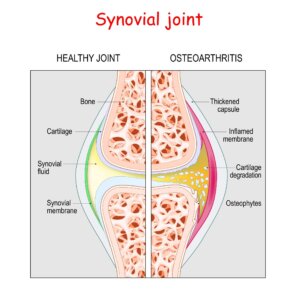 The joint has a nice tough outer lining called a capsule and inside this lining, a thinner lining exists called a synovial membrane (synovium). The membrane does two things. First, it ensures that the joint is balanced chemically. It provides nourishment to the cartilage and keeps it healthy. If the synovium is healthy, the joint has an excellent chance to remain in good health.
The joint has a nice tough outer lining called a capsule and inside this lining, a thinner lining exists called a synovial membrane (synovium). The membrane does two things. First, it ensures that the joint is balanced chemically. It provides nourishment to the cartilage and keeps it healthy. If the synovium is healthy, the joint has an excellent chance to remain in good health.
While diseases are directed at this critical part of the joint, as in rheumatoid arthritis and gout, to name but a couple of the common arthritides, injury can also affect the synovium.
X-rays
If your clinician orders an x-ray for the toe joint, this mainly help to show how much joint space is present or lost. The excess bone produced (osteophytes) can provide a gauge of deterioration. The other feature used in the x-ray is identifying bone density or bone loss. As we age, our bone thins, but feet are not used to gauge osteoporosis, whereas the spinal vertebrae offer a better indicator.
The cartilage is not visible on an x-ray and specialised scans called MRI (magnetic resonance image) or CT (computerised tomography) are required to evaluate deeper levels of damage. Ultrasound may help with soft tissue but not bone.

Footeducation deals with surgery mainly but it is a great site for video material.
Lubrication
Cartilage (hyaline) works with a joint that produces a thick fluid that is clear in colour and made of synovial fluid. The fluid contains hyaluronan (hyaluronic acid) manufactured by the synovial membrane. The cartilage surface has a slimy material (glycoprotein) similar to the secreted sticky trail left by snails. It is wonderful in reducing friction as the toe and bone (metatarsal) compress, twist and slide, watery content leaks from the cartilage in one direction and returns later after pressure has reduced. But, of course, this happens all of the time.
Provided that cartilage is intact, the lubrication mechanism works well. However, if the surface is damaged, the mechanism fails to work.
Cartilage has layers
The top layer (lamina splendens) is essential and allows water to pass back and forth during activity. Deeper layers are arranged differently from top to bottom. At the bottom, the cartilage cells (chondrocytes) start to become bone, called the tide mark. Below this, the bone has a blood supply. It is essential to realise that cartilage does not have a blood supply and relies entirely on the synovium for nutrients (foods). Waste and breakdown products are removed from the synovium.
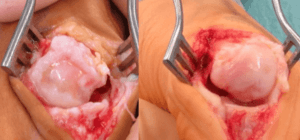
Damage
If the cartilage is damaged down to the level of bone, bleeding will occur in the joint. The synovial fluid will change colour and can form small clots forming scar tissue. If you stub your big toe (turf toe), the softer tissue is damaged first. If the damage is significant, or you just keep repeating that damage, then the changes in the joint deteriorate. New bone may start to line the joint, and the joint does not work when that happens.
Hallux rigidus

clinical observation of osteophytes are not hard to spot and cause callus, skin damage and pain from shoes
If your joint movement reduces, the synovial fluid cannot flush debris away intended. The joint dries out and becomes rough, and splits. In other words, it ages very fast. Once the joint becomes rigid, the synovial membrane is irritated by bony outgrowths (osteophytes).
The damage continues and in effect, extensive bone outgrowth also damages the capsule. Pockets of fluid can escape with pressure, forming a fluid pouch (ganglion).
This can arise on the side and top of the joint. HR is illustrated by the widening of the joint (see earlier x-ray).
Hallux valgus
left hallux rigidus with valgus and right hallux valgus. This emphasises the limitations of osteophytes as projections over joints. The damage is far greater in the left hand picture
One of the big problems with hallux valgus is that it may start as a mild deformity and then enlarge later. This is because a separate part of the joint is compressed; the joint surface has no pressure, so it thins anyway. We know that to keep our skeleton healthy, including bone and joints, we need stress to sustain the substance. This is why the weightless nature of space is bad for astronauts, as tissues (bone, joints, muscles) can waste away without the benefits of earth’s gravity.
As the joint deformity increases in HV, the surface and parts of the cartilage become eroded. The side, centre and underneath the joint are affected more frequently. But the curious fact is that unless the surface reaches the bone, it copes well enough unless the synovium is damaged.
Once movement stops, the combined effects of bleeding and inflammation accelerate both more internal damage and cause pain. Most people do not suffer joint pain from HV, but they do for HR.
Treatment
- Pain medication is but temporary and acceptable for an acute injury. You hurt yourself, find that you cannot walk and take pain medication and that’s fine.
- Manage the swelling with ice packs and avoid exercise for a few days. If the pain lasts beyond 5 days or the toe joint is swollen, seek advice. In children, toe joint damage is more critical as it can split the joint damaging healthy development and even affecting growth. Cartilage can repair in children up to a point, but not in adults. Cartilage is not like bone which is repaired with the same material. Instead, cartilage fills in with scar tissue.
- For hallux valgus joint pain, use night splints to align the joint. This will not change the position quite as adverts suggest, but it will help relieve pain. Plaas (2020) in Germany undertook some research, and their system is now available. Cheaper systems do exist but this is well designed and can be used in weight bearing.
- Use a stiff-soled shoe to reduce movement for both HR and HV where there is joint pain.
Should you use glucosamine tablets, and do they work?
There is no doubt that glucosamine (sugar-protein) is part of normal joint chemistry, but it does not have a proven scientific value in working for everyone. However, the general view is to try it as it will not harm. In much the same way, Vitamin D helps but is not the whole answer.
Injections
Corticosteroid
A steroid injection that acts as an anti-inflammatory will help the synovial inflammation. This is what you need to know. One injection is recommended; if it does not work, do not repeat it. Repeating steroid injections will also damage your joints. With HR, Grice (2017) found that 92% of patients benefitted initially, but by 2 years, the effect had dropped to 9%. Without HR joint pain can be relieved more effectively with steroid injections, but again these should be limited to single injections.
Hyaluronic acid (HLA)
While glucosamine is not a proven benefit, directly injecting a similar chemical product can assist in some cases. Again, studies have mixed results, but it is an option you can discuss with your clinician.
Laser treatment
External influence on the joint from low-level laser therapy can be beneficial and probably works in the synovium. Sufficient evidence in human studies associated with the first toe joint is not available at present.
Surgery
- Joints that no longer work, are constantly painful and fail to respond to conservative treatment may respond to surgery.
- Hallux rigidus: Joint replacement (arthroplasty) can be offered, or the joint can be made stiff (arthrodesis).
- Hallux valgus: Correcting the alignment of the joint is achieved by making the bone fit better by making a particular cut or taking a wedge (osteotomy).
Conclusion
Arthrosis is a general condition and this article has covered the basics of joints and how damage changes movement. The two features of doom joints are the development of extra bone (osteophytes) that block joint action, inflammation, and changes in the synovium (synovitis), and vital for normal cartilage health. Arthritis due to these changes is known as degenerative arthrosis. At the same time, osteoarthritis (arthrosis) affects larger joints such as the hip and knee and is related to genetic trends and weakness within the cartilage.
Rheumatoid arthritis is complex, but the primary damage is an autoimmune process. Damage arises due to abnormal white blood cells attacking the synovium. Gout is where the chemical balance associated with excretion through the kidneys fail. Deposits of white chalky material affect the synovium. The lubrication mechanism fails and the joint cartilage dries out.
The joint specialist is a rheumatologist and many modern drugs help reverse some of the chemical problems within the synovium these are called disease-modifying medicines or DMARDS. However, the subject of rheumatology is complex and overlaps with medical issues, e.g. diabetes and thyroid hormonal imbalance.
In feet, the big toe joint can be managed conservatively and by surgery by podiatrists who specialise in foot pain, alignment and changes in the tissue as a result of injury or medical disease.
Podiatry has been established in many countries, but the best known include the USA, Canada, UK, Spain, Australia, South Africa, Israel, New Zealand, Holland, Finland, Mexico, Hong Kong, Singapore and some Middle East countries. In other European countries, the scope, training and service may vary, but podiatrists (podologues) have expanded. Chiropody is a term used by older podiatrists but is not a degree subject in the UK, Australia or USA. In the USA all podiatrists use the prefix ‘doctor’.
David Tollafield is a former podiatric surgeon based in the UK who has written extensively on the foot and lectured widely worldwide.
You can read other articles covering the big toe on this site:
- Hallux Valgus, known as bunion
- What age is best for bunion surgery?
- Common forms of foot arthritis
- Toe shape causing a nerve pain
- Medically related painful toes
You can now read other stories about the foot from the same author. Available from Amazon books
Thanks for reading “Arthritis and the Big Toe” by David R. Tollafield
Last reviewed September 2023
Published by Busypencilcase Communications. Est. 2015 for ConsultingFootPain



Recent Comments