What to do when things are not quite right?
This series covers different patient stories taken from their own words. All had stiff big toe joint pain. This is Tom’s story When things don’t go to plan and what do you need to know? Blue writing will take you to different links and help build a picture depending upon the detail you need. Throughout, clinician comment will elaborate on the storyline. Please read the other cases on ConsultingFootPain as these paint a different picture starting with the Introductory article.
I joined Tom two months after surgery in a UK National Health Service Hospital. Tom was 80 at the time of surgery.
The prosthetic joint
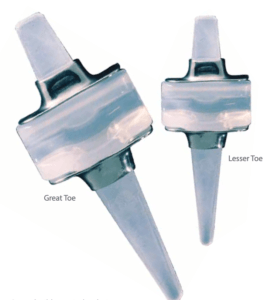
Swanson implant (silicone) C/O Wright Medical
Tom’s first saw an orthopaedic surgeon for a trigger finger but complained about his big toe as well after being asked if there were any other problems? He ended up talking about his left big toe to the surgeon.
“I took my shoe off and he said,”
“Ah, classic hallux rigidus,” or whatever it is. And he said, “I’ll tell you what. I’ll do that at the same time as I do your trigger finger. I could fuse it, but it’d be much better to have a replacement silastic joint. It’ll give you more movement, and that’s what I recommend. I didn’t think anything at all but it was beautifully casual. You walked yourself into the operating theatre and you climbed up onto the bed, before the anaesthetist got to work. Anyway, it was very successful and it was great for about 12 years and then it began to hurt. And for the last couple of years I couldn’t walk properly. I had to walk on my heel on the outside of my… to try and protect the toe. After playing a round of golf it hurt like hell, sort of about the 15th 16th hole and then it got to the stage where I couldn’t play 18 holes.”
CLINICIAN COMMENT
The clinician often does not know his treatment has a limited shelf life. The implant, in this case a silastic implant had lost its value. (Rachel’s case is the reverse of Tom’s story). The most common problem with silastic implants is when the hinge tears and compresses losing any functional value. The use of a metal washer (grommet) helps minimise this. The manufacturer advises 10 years life-span. I have seen these last 7-20 years. They can be replaced with a second spacer. Leaving the implant to over age 55-60 means the implant does less work as activity reduces. Spacers and joints therefore have a limited life-span. Because many foot surgeons are not happy with the unpredictability of prosthetic implants they offer a stiffening procedure. This is called an arthrodesis.
Seeking a second opinion
Tom sought a second consultation with a different surgeon. Revision surgeries are not always easy. He said, “This is a tricky procedure because I’m going to have to do a bone graft, and I’m also going to have to do a skin graft because there won’t be enough skin.” he had to lengthen the toe as it had shortened. Tom asked “Why can’t you just amputate the toe?” The surgeon did not recommend this.
CLINICAL COMMENT
Amputations of the great toe should only be undertaken when all other methods cannot be performed. The indications for amputation fall broadly into three categories. Loss of blood supply (ischaemia), cancer (proven malignancy) and non-healing (infection of bone). An additional category could include unremitting pain but rarely in the case of diagnosed complex regional pain syndrome.
Constant pain in the big toe
“Another year went by and it got more painful and I went back to the GP and he sent me to a different man.” He reiterated again to Tom that it was a tricky procedure, there would be the bone graft and the skin graft etc. “So I accepted that I wasn’t going to do anything about it for a while and I did in fact seek a third opinion. Now the consultation was slightly different. The later surgeon (NS) said to me, I don’t think it’s necessary to lengthen the toes. I don’t have to do a skin graft, and I’m fairly confident that you will be pleased with the outcome.” He explained everything that could go wrong. Curiously the surgeon said, “I’ve never had an operation myself, and I never want one because I know what can go wrong.”
CLINICIAN COMMENT
Consent will be discussed at the end and it will become relevant. We need to explain bone lengthening and skin grafts.
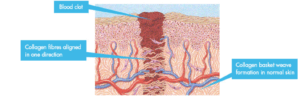
Revision surgery is always riskier because scar tissue damage builds up. Scar tissue is made up from fibrous material called collagen and tethers around nerves, blood vessels and ultimately sticks to cartilage and joint linings. Physiotherapy (self or professional) assists rebuild the movement after surgery. The toe can shrink in length and so functionally fails to work as it once would. Building the missing gap with bone is important and traditionally this comes from the pelvis. The iliac crest offers the best quality and as it comes from the patient offers the best bonding. If the toe lengthens the skin may become over tight and skin supplement may be required. For a toe in general this is not necessary unless the shortening from the original surgery was extensive.
Planned surgery goes ahead
 Tom went ahead after taking multiple opinions. His surgery included a bone graft taken from the hip.
Tom went ahead after taking multiple opinions. His surgery included a bone graft taken from the hip.
“Up until probably two weeks ago, I regret it very much doing it because NS impressed upon me how incredibly important it was to keep the foot elevated for 15 minutes out of every hour. And I did find that difficult to cope with, lying on your back with your foot up. And then the pain level was worse… If ten is bad, naught is no pain at all. Before I went, after I’d done some activity like trying to play golf or mowing the grass, it would be seven out of ten, and it would last most of the night. keep me awake and it would get swollen. After I had the operation it was for the first two or three weeks it was sort of seven all the time. And then then it became about five, I suppose five out of ten.”
Tom was followed up at 6 weeks with x-rays and advised to stay in his rigid shoe. A registrar saw Tom and explained that his consultant NS had to dig around a bit more than expected to remove the failed joint. Based on this he said “it’s going to take a bit longer, which I was a bit disappointed with.” Later NS told Tom that the plastic had destroyed some of the bones.
“I needed more time, and would be seen again in three months, which was last week. I tried putting a shoe on and found I could just get one on. And it began to feel better. The x-ray showed that the bone had knitted together satisfactorily. It was a big, big plate. The plate they put in covers the whole length of the wound. It’s about four inches, I would say, and it had a lot of screws in it. I was amazed how many screws it had. I think there were at least four on each side. There were about eight screws in the whole thing.”
The surgeon was satisfied all had gone together well and advised that Tom would not do any harm, and could start doing normal things. “I played two nine hole and the discomfort was a bit less than it was before I went to have it done. And right now, the pain is two or three out of ten. I’m aware of it, but it’s not bad. I find in the morning when I wake up, the pain is zero. When I wake up in the morning, there’s a nice gap between all my toes, and at night time when I go to bed – particularly if I’ve done something – it’s swollen, and there’s no gap between toes. I asked the guy when I saw him if that was anything to worry about.” Tom was told me that he had at least another nine months before he would get the full benefit.
CLINICIAN COMMENT
The time for recovery and returning to normal life is the gauge most people use to judge success. What is recovery? When is normal, normal? We are talking arthrodesis fusion. That is sticking the ends of two bones that normally move so they bond as one. Bone healing of a fracture can take anywhere from 6 weeks to 4 months. The plate is a bar with holes made from metal (stainless steel or titanium). Screws fit through the holes and the bar prevents the toe from moving and allow earlier return to function. Six to 8 weeks, therefore, is reasonable as the bone is braced. A walker cast helps create earlier movement. Plaster and plastic cylinder casts are no longer as popular hence why plates are chosen. Walking helps reduce some swelling while overuse increases swelling. Contours are lost and footwear is difficult and ultimately may need to be changed to fit the new foot. A cautious surgeon would play to the longer side of recovery to prevent patients from becoming despondent. Delays through the inability to drive, walk, return to work, are seen as negative so realistic goals are vital. Six-nine months is a sensible recommendation. Swelling can last for 4-6 months easily and sometimes there is a permanent swelling. This is not necessarily abnormal. The foot can suffer discomfort in cold and the hardware (plate/screws) seem to conduct a different sensation than when the weather is warm.
Tom pointed out that his thigh was giving him problems
“it’s nasty and it feels as if the skin has been burnt. It’s a bit like a shingles pain, but it tends to be only when you touch it. Most of the time, I’m unaware of it, it’s just touching it.”
CLINICAL COMMENT
Tom’s surgeon advised massage but he wanted to know where to massage and how to do it. Massaging scars is an important consideration and can help to desensitise wounds. Surgeons, however, are not always the best to advise and for my money, the physiotherapists we referred to were better as they were more in tune with the patients need. I listened to them and backed them up. Some (foot) surgeons do not place enough importance on simple things like rehabilitation. Tom’s thigh pain would subside and would almost certainly be due to muscle and local nerve bruising as the thigh is compressed under a pressure cuff to stop blood flow during surgery. I have seen this a few times and although not common it may be due to longer periods than 45 minutes when the muscle and nerves are more vulnerable to both pressure and oxygen depletion.
Consent

https://www.dreamstime.com/photos-images/signing-consent.html
By 2010 consent has received much debate and standards had improved from 10 years earlier. This is important because it constitutes a contract of agreement. The patient gives the surgeon permission to undertake physical harm based on delivering benefits. Consent is where things can go wrong. Most surgeons will have had a complaint or even had to defend their actions based on the misunderstanding over what was said and what risks were provided. It may not surprise the reader that this area of our work is the most hotly contested. As a patient myself, and a retired foot surgeon, I am only too aware of the uneven triangle (see the triangle of consent below) that we find ourselves in.
When were you asked to sign your consent?
“I was asked to sign a consent form in the clinic, which I did. He was very blunt and honest about everything that could go wrong. He told me about deep vein thrombosis and that I could die and if everything went terribly wrong I could get a lot of infection. I might lose my foot, he said. “I didn’t feel he was putting any pressure on me to do it. but he did give me confidence.”
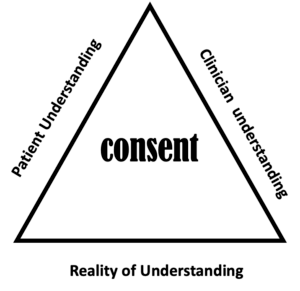
(C) ConsultingFootPain (2021). Consent has three sides to the process.
CLINICAL COMMENT
Tom’s consent was good in that he recalled some of the big points made. There may have been one or two matters left off. Here is a checklist of what was included. The words in black are added areas that should or would have been added.
- Loss of life through an unknown medical emergency. This is mercifully rare.
- Overwhelming infection can lead to the loss of a foot, or limb and even result in death. Of course, since Covid-19, matters have changed approaches to surgery.
- Deep venous thrombosis is a clot usually in the calf and is fully treatable. On rare occasions, a clot can fly off to the lung (pulmonary thrombosis) and is life-threatening.
- What is often not mentioned is numbness and nerve damage.
- Overwhelming pain can be caused by a rare and unusual problem called complex regional pain syndrome.
- Slow healing is not uncommon with big toe surgery, although, for the most part, it may only affect a small length of the wound.
- Scar tissue causes nerves to be bound down with some tenderness with a light touch.
- Hardware removal due to movement or breakage, or allergy.
All surgeries have an element of concern, and between 2010-14 this author implemented a risk scale of 1-5 based on the impact rather than the actual percentage risk of a post-surgical problem.
Two years on and follow up
 I approached Tom in April 2021 to see how things had gone. My questions were listed as follows,
I approached Tom in April 2021 to see how things had gone. My questions were listed as follows,
- Have you had any setbacks since surgery on either foot?
- Has the procedure solved your problems?
- Are there any activities that you cannot pursue where once you had engaged in those same pursuits?
- Is there anything you would like to add to your story?
Tom launched into a dialogue that will form the next article as we await what his consultant has to say. Armed with a referral from his GP it will be interesting to see how long it takes to be seen. Downsides of arthrodesis fixation
Thanks for reading ‘Big toe pain and Tom’s story’ by David R Tollafield
A Behind the Scenes Patient Journey Series
Why not read more about the bunion (hallux valgus) and behind the scenes on this website or buy the e-book/paperback by the same author?

Published by Busypencilcase Reflective Communications Est. 2015
4th July 2021

Trackbacks/Pingbacks