‘Feet and safety at home’
Welcome to ‘feet and safety at home’ responding to injury (Part 1)
When it comes to accidents we all know safety in the home is important but what we don’t know is how often feet contribute to injury. Australian Podiatrist Hylton B Menz has written extensively on falls in the elderly but the effect and data is not something we can easily locate.
If we want to know about the effects of home activity we could look at The Royal Society of Prevention of Accidents or RoSPA as it is better known. This organisation publishes statistics on all kinds of accidents. However, feet tend not to be so well recorded. As far as home is concerned feet and safety are not easy to tease out from any published data.
In general, though we recognise common accidents relate to a variety of conditions such as splinters and debris injuring the skin,. Then there are falls or sharp implement injuries. Poor placement of ladders. Accidents from using tools incorrectly and then lifting heavy materials causing back injuries. When it comes to feet and safety at home these two significant parts of the anatomy to easily lead to a disaster.

Click here for an edited audio version
Falls at home
 As a category falls probably climb to the top of the ladder as far as incident frequency. Perhaps more so in the older population. This might be understandable. As muscles are used less as we age, the messages informing our brain slow down. This whole aging process is not helped by muscle wasting (atrophy). The nerves tell our brain how to move using ‘feedback’ information from the tendons and tension. Together with our reflexes the system work slower compared to when we were younger. See article (break a leg!) As we age we find that it is less easy to adjust so that sways and tilts turn into that nasty off-balance effect. Add in tinnitus, congestion, infections in the inner ear and the risk of falling is compounded.
As a category falls probably climb to the top of the ladder as far as incident frequency. Perhaps more so in the older population. This might be understandable. As muscles are used less as we age, the messages informing our brain slow down. This whole aging process is not helped by muscle wasting (atrophy). The nerves tell our brain how to move using ‘feedback’ information from the tendons and tension. Together with our reflexes the system work slower compared to when we were younger. See article (break a leg!) As we age we find that it is less easy to adjust so that sways and tilts turn into that nasty off-balance effect. Add in tinnitus, congestion, infections in the inner ear and the risk of falling is compounded.
While we can treat arthritic joints and apply physiotherapy to strengthen muscles, we should exercise regularly. In fact, regular exercise is well proven as a method to keep us supple. People who visit my local gym are often several decades older than me. Unlike the younger attendees though, the older user appears more sensible. This means that they push their bodies at a slower pace.
Accidents in younger people
When it comes to younger people falls are often due to lack of care. We can all fall on slippery surfaces. That trait called a failure to concentrate on a physical activity is common. Not watching where we are going of often the perpetrator of distracted attention. Going over on one’s ankle is easily done.
 When my stepson sent me a picture of his friend’s effort to mow the lawn, he was taken with the fact it was not just the grass that his friend was trimming. His friend managed to sever a few toes as well at the same time. Lack of concentration? Well, yes, but he was not wearing sensible shoes. In fact, he was wearing sandals. Rotary mowers are unforgiving when it meets flesh!
When my stepson sent me a picture of his friend’s effort to mow the lawn, he was taken with the fact it was not just the grass that his friend was trimming. His friend managed to sever a few toes as well at the same time. Lack of concentration? Well, yes, but he was not wearing sensible shoes. In fact, he was wearing sandals. Rotary mowers are unforgiving when it meets flesh!
Of course, as a podiatrist, this was not something I was called on to fix as it was emergency medicine and ideally a plastic surgeon would be called in if one is lucky. If not, it is amputation, debridement and weeks of dressings and hope that infection does not set in.
The Sharp Object & the shoe
 Being the paragon of common sense I select the right footwear for the right job. In this case my old trainers for doing those odd jobs like fixing the shed roof. The galvanised tacks are covered with a heavy residue of tar as they penetrate the softer material compressing the roofing felt to the wooden under the structure.
Being the paragon of common sense I select the right footwear for the right job. In this case my old trainers for doing those odd jobs like fixing the shed roof. The galvanised tacks are covered with a heavy residue of tar as they penetrate the softer material compressing the roofing felt to the wooden under the structure.
A sharp object can easily fall to the ground as it bounces out of the felt. Left to fumble for a spare tack kept in my trouser pocket avoids having retrieved the tack. These tacks can be anything from ¼ to ¾inch in length and so if you are unlucky the tack point side up can penetrate the outer sole; and it did.
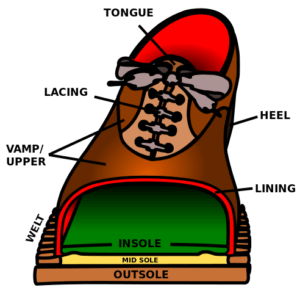
If the outer sole is thin and if the midsole (see the diagram cross-section of the shoe above) is not robust, a tack can run right through entering the foot piercing the skin like butter (video clip). This actually happened to me and you can read about it if you click the link.
A typical foot injury at home
 A penetrating injury, not like the cover picture hopefully, should be stopped by a decent shoe. If not the damage done by a nail, tack or foreign body will enter the skin. Dirt, and in my case tar, as I was hammering roofing felt in, could penetrates the skin. Despite limited bleeding the depth of the penetrating injury now poses a risk of infection. I can only say in my defense that quality shoes saved the day. The tack failed to penetrate beyond the midsole.
A penetrating injury, not like the cover picture hopefully, should be stopped by a decent shoe. If not the damage done by a nail, tack or foreign body will enter the skin. Dirt, and in my case tar, as I was hammering roofing felt in, could penetrates the skin. Despite limited bleeding the depth of the penetrating injury now poses a risk of infection. I can only say in my defense that quality shoes saved the day. The tack failed to penetrate beyond the midsole.
My wife is seen removing the nail in the video, but I have removed her sounds of frustration from the clip (I hope) with my own voice, but she does a good job with a penknife which in itself looks precarious. You can also click here to see what might be best in a First Aid Kit

In my next article I provide some guidance on what to do with various penetrating injuries using my own experience. Part 2 Self Help
Medically challenged patients would be best registering their injury with a local doctor (GP) or clinic nurse or call 111 only use A&E and 999 for life threatening conditions
Why not sign-up and stay in touch
Thanks for reading ‘Feet and safety at home’ by David Tollafield.

First published 5th September 2019. Re-issued as a two part article July 2020
Please also listen to the audio version
Published by Busypencilcase Reflective Communications Est 2015
![]()

Recent Comments