Poor data collection exposed
Unravelling the impact of a pandemic
Poor data collection was exposed if the author’s findings bear truth in this report using the Royal of College of Podiatry’s data base. Tony Maher, consultant podiatric surgeon and audit analyst for the college provides his latest figures comparing data from 2019 to the period of the pandemic taken from the official government statistics or HES. (Editor)
![]()
Maher, A. The Potential Effect of Poor Data Collection on Podiatric Surgery and Patient Care highlighted by the Corona Virus Pandemic. Podiatric Reflective Practice. ConsultingFootPain/Busypencilcase Reflective Communication. 2021; April:1-6
Elective surgery within the UK’s healthcare system including that provided by podiatric surgeons has been affected by the pandemic which was recognised during early 2020. Using data collected by the College of Podiatry Audit System, PASCOM-10 (College of Podiatry 2020, Tollafield DR, 1994, Rudge G, 2003) the author has been able to identify notable anomalies likely to add to the long term effect on post-Covid recovery in the UK when applied to podiatric surgical service delivery. Understanding the impact on podiatric surgery is difficult to fully assess because data is collected by acute trusts in hospital or day surgery settings with different interpretations over how to code the source of delivery. NHS Digital produces a number of detailed reports on both inpatient and outpatient activity in English Hospitals referred to collectively as Hospital Episode Statistics (HES) (England NHS, 2021). Where podiatric surgery services are provided in non-traditional surgery settings, and importantly hosted by community healthcare trusts or social enterprises, that activity is not captured by the HES datasets. At a local level, provider trusts can work with their commissioners to understand the impact of COVID-19 on service delivery and can accurately identify waiting times. At a national level PASCOM-10 and HES data provide options for understanding the wider impact of COVID-19 on podiatric surgery activity.
Does the college clinical database answer our primary question?
How reliable is the HES data and how does it compare to our own College data base used by 80.6% of podiatric surgeons in England (2019)?
The PASCOM system prompts users to input data relating to demographics, surgical procedure, and associated medicines together with pre- and post-operative outcome scores using the Manchester-Oxford Foothealth Questionnaire (Dawson J, 2006). Patient satisfaction is also captured following surgery. Once uploaded, the 99 departments who contribute to the dataset can then be analysed by designated officers on behalf of the College of Podiatry. Data is anonymous and reports are not identifiable by name. All centres must seek local ethical approval for use of PASCOM as a clinical audit tool from their respective trusts and centres. Since 2010 raw data reports have been published (Information & resources, 2021). This information provides an insight into both uptake of the audit system and more generally the prevalence of podiatric surgery in England. Data relating to nail surgery and steroid injections have been filtered out. NHS Digital reports on patient activity collectively known as Hospital Episode Statistics (HES) and provides a detailed dashboard which can be interrogated (NHS Digital, 2021). Both Podiatry and Podiatric Surgery are listed on the dashboard and this was identified for the period April – November 2020 and compared with data from the College database.
Centres bundled together
Podiatric surgery is conducted either in the acute sector within a formal hospital setting, or it may be carried out in a dedicated community centre. Additionally NHS services are offered as part of NHS Choose and Book at commissioned independent hospitals and dedicated centres. For the year Jan-Dec 2020 admissions for surgery reduced by almost 56% when compared to the same period in 2019 (Table1) according to data collected by the College of Podiatry. Podiatric activity occurred in 99 centres, 88% of which provided NHS care. Community-based services accounted for 51.8% of NHS treatment with the remainder provided by either acute Trusts or NHS Choose and book in the independent sector. When comparing HES data between April – November 2020 a similar trend existed. Overall day case admissions were down by 42.5%. For cases designated as podiatric surgery and podiatry both had dropped by 81% and 62.9% respectively compared to the same period in 2019.Looking at (acute) admissions for podiatric surgery where 300 admissions were recorded for a normal month, the drop was more dramatic reaching a low of just 16 admissions in April but recovering in October at 142 admissions. Outpatient attendances were also affected with an overall reduction of 25.6%. Podiatric surgery saw a reduction in outpatient attendance of 56.4% whilst podiatry saw attendance reduce by 49.1%.
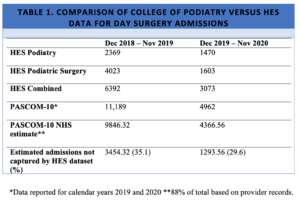
*Data reported for calendar years 2019 and 2020 **88% of total based on provider records.
The long Covid effect on service delivery
The NHS has been affected in different ways and will continue to be under considerable pressure for some time. Many elective services stood down resulting in some 4.42 million people left waiting for elective surgery. Halting elective surgery is not without consequence. Patients will now face unprecedented delays in receiving care as services gradually return to normal capacity. At the time of writing, many podiatric surgery units remain stood down and their teams redeployed.
The NHS has been affected in different ways and will continue to be under considerable pressure for some time. Many elective services stood down resulting in some 4.42 million people left waiting for elective surgery. Halting elective surgery is not without consequence. Patients will now face unprecedented delays in receiving care as services gradually return to normal capacity. At the time of writing, many podiatric surgery units remain stood down and their teams redeployed. When services are restored, long waiting lists will require careful prioritisation to ensure those with greatest need are cared for appropriately. Elective surgery may, by definition, be entered into by choice, but such patients will be living, in the case of podiatric surgery with chronically painful musculoskeletal complaints. It is recognised that patients with chronic foot and ankle complaints suffer significantly impaired health related quality of life (Gilheany, M, 2008, Maher, A, 2011). On top of this we know from our college data that many patients are of working age. In the most severe cases chronic foot pain will make it difficult for patients in some industries to remain economically active. People also tend to stop or reduce exercise participation when significant foot pain develops. Improvement in mobility is a central outcome expected for podiatric surgery (Wilkinson, 2011). It is important that we do not ignore the wider societal impacts of longer waits for treatment.
COVID-19 will also cause long term problems for our more vulnerable patients and their recovery from eventual surgical treatment. Prolonged periods of lockdown and shielding will have resulted in significant physical deconditioning for some. The direct impact on mobility associated with lockdown frailty will make recovery from surgery all the more difficul (de Biase, 2020). NHS England must ensure patients who have already experienced the longest waits of a generation are not simply forgotten when recuperating from surgery. Failure to address this need when normalisation is restored will result in ongoing deconditioning and loss of physical health which will give rise to further societal costs.
HES data captured when podiatric surgery admissions and outpatient attendances are recorded in NHS hospitals underestimate the true extent of podiatric surgery in England. The College of Podiatry records podiatric surgery by podiatric surgeons for 88% of surgery originating in NHS centres. Comparing the two datasets it appears that around a third of NHS podiatric surgery admissions go unrecorded by NHS Digital in their HES dataset. Such analysis suggests that podiatric surgery provided for chronic foot pain is under represented. The net effect would be to skew interpretations for determining the economic impact on the need for patient care and accurate planning for future provision of foot health services. There is also a need for clarity as to what constitutes podiatry and podiatric surgery within the HES, data capture recorded for NHS Digital. There is confusion about the two terms, podiatry and podiatric surgery and when to apply them in hospital coding.
The dramatic reduction in admissions captured by the College of Podiatry’s database PASCOM-10 and compared to NHS Digital HES database, has identified significant discrepancies between admissions recorded by the two systems. It is apparent that the true extent of NHS podiatric surgery is currently under reported by Government systems and this should be addressed as a priority.
Next month the editor follows up with an interview with Tony Maher looking at the scene behind the data collection – challenging NHS evidence.
![]()
- College of Podiatry. PASCOM 10 – The Podiatry Audit Tool. http://www.pascom-10.com/. Published 2020. Accessed April 15, 2020.
- Tollafield DR, Parmar DG. Setting standards for day care foot surgery . A quinquennial review . Part I. Br J Podiatr Med Surg. 1994;6(1):7-20.
- Rudge G, Tollafield D. A critical assessment of a new evaluation tool for podiatric surgical outcome analysis. Br J Pod. 2003;6(4):109-119.
- Information & Resources. https://www.pascom-10.com/information-resources. Accessed February 7, 2021.
- Hospital Episode Statistics for Admitted Patient Care and Outpatient Data – NHS Digital. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-episode-statistics-for-admitted-patient-care-outpatient-and-accident-and-emergency-data. Accessed February 7, 2021.
- Dawson J, Coffey J, Doll H, et al. A patient-based questionnaire to assess outcomes of foot surgery: Validation in the context of surgery for hallux valgus. Qual Life Res. 2006;15(7):1211-1222. doi:10.1007/s11136-006-0061-5
- Gilheany MF, Landorf KB, Robinson P. Hallux valgus and hallux rigidus: a comparison of impact on health-related quality of life in patients presenting to foot surgeons in Australia. J Foot Ankle Res. 2008;1:14. doi:10.1186/1757-1146-1-14
- Maher AJ, Kilmartin TE. An analysis of Euroqol EQ-5D and Manchester Oxford Foot Questionnaire scores six months following podiatric surgery. J Foot Ankle Res. 2012;5(1):17. doi:10.1186/1757-1146-5-17
- Wilkinson AN, Maher AJ. Patient expectations of podiatric surgery in the United Kingdom. J Foot Ankle Res. 2011;4(1):27. doi:10.1186/1757-1146-4-278.
- de Biase S, Cook L, Skelton DA, Witham M, ten Hove R. The COVID-19 rehabilitation pandemic. Age Ageing. 2020. doi:10.1093/ageing/afaa118
Additional references
- https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-to-covid-19-letter-simon-stevens.pdf. Accessed February 7, 2021.
- Statistics Consultant-led Referral to Treatment Waiting Times Data 2020-21. https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/rtt-data-2020-21/. Accessed February 7, 2021.
Thanks for reading ‘Poor data collection exposed’ by Antony Maher

Published by Busypencilcase Reflective Communications Est. 2015
16th April 2021

Recent Comments