John’s four-month journey
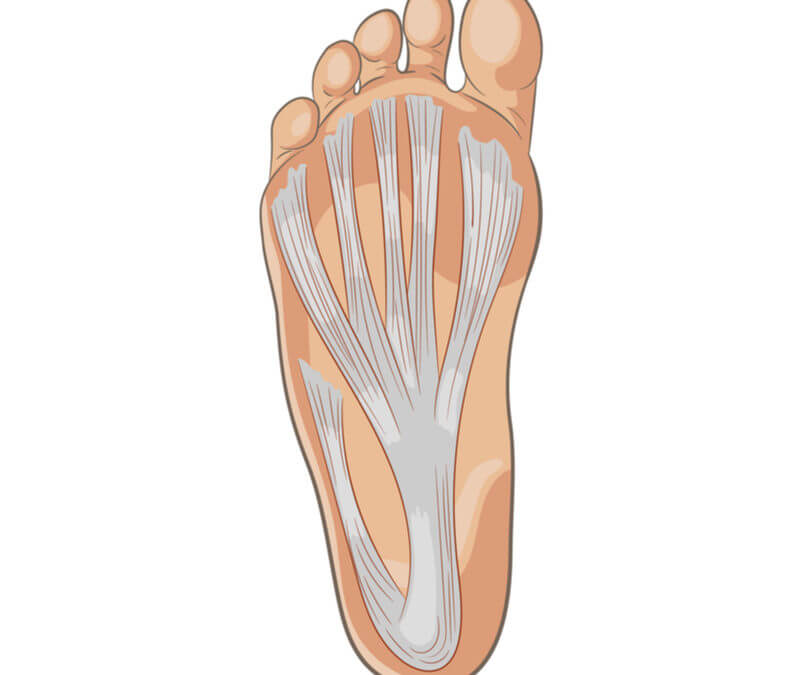
 John was a 47-year-old patient who agreed to keep a diary after an operation on his chronic plantar fasciitis. Many reading this will shake their heads negatively – of course, this is not necessary as we can treat PF conservatively. The story came about in 2017 after much conservative discussion was carried out. The idea of a heel spur of course was discounted as the myth it really is. I admit to undertaking spur surgery as trained, but that was years ago, and having reflected on my surgical outcomes, recovery was far too long and traumatic. It seemed crazy that I had trained using a minimal incisional surgery technique – meaning a tiny keyhole or MIS. You needed a large number of cases to justify the investment and my heel pain surgery group represented less than 5%. We used cadavers, when training, and optic fibre guides (endoscopes) originally, but my NHS Hospital was not buying the kit and neither was the private sector. In reality, most heel pain and that including PF can resolve with other, more modest techniques. Larsen (2019) undertook a small study and appears to have used bone spur resection. This is something I would no longer advocate based on my experience of fascial release alone. Unfortunately, only small numbers are cited because surgery for PF is truly not needed often.
John was a 47-year-old patient who agreed to keep a diary after an operation on his chronic plantar fasciitis. Many reading this will shake their heads negatively – of course, this is not necessary as we can treat PF conservatively. The story came about in 2017 after much conservative discussion was carried out. The idea of a heel spur of course was discounted as the myth it really is. I admit to undertaking spur surgery as trained, but that was years ago, and having reflected on my surgical outcomes, recovery was far too long and traumatic. It seemed crazy that I had trained using a minimal incisional surgery technique – meaning a tiny keyhole or MIS. You needed a large number of cases to justify the investment and my heel pain surgery group represented less than 5%. We used cadavers, when training, and optic fibre guides (endoscopes) originally, but my NHS Hospital was not buying the kit and neither was the private sector. In reality, most heel pain and that including PF can resolve with other, more modest techniques. Larsen (2019) undertook a small study and appears to have used bone spur resection. This is something I would no longer advocate based on my experience of fascial release alone. Unfortunately, only small numbers are cited because surgery for PF is truly not needed often.
Surgery on reflection
The aim of this article is to review the diary of a patient prospectively as part of reflective practice. The links to the articles above recommend at least six months of treatment first. I have drawn on two papers Larsen (2019) and Ali (2021) to reflect current thoughts. Many papers can be found dating back to 2000 when the endoscopic technique started to become popular. The reader is reminded that there is no single fix for PF. Much of the success comes down to occupational changes. Even I found this out when hitting the treadmill earlier in 2021 sustaining a bruised heel. The message was and still is look at causative factors. And so we meet John and his chronic heel pain. Consent was taken at a point when we agreed he was desperate. Do look at some of my other articles including managing PF with stretching.
Surgery for Plantar Fasciitis: a last resort
Past medical history (using John’s words)
After undergoing a 97% blocked carotid artery operation in 2010 and spending 3 months convalescing, I found I had severe pains in both feet when I returned to work. I consulted my GP who diagnosed Plantar fasciitis, then came an array of physiotherapy, walking aid insoles, stretching exercises, and even electrotherapy bombardment to both feet/heels. This continued for 6 years with no or little relief until my GP referred me to see David at his Hospital. After my first consultation, it was agreed that steroid injections may relieve the pains and these were done sometime later. The steroid injection worked in the right foot but not the left. As there wasn’t any improvement and now I was starting to limp more aggressively as walking was beginning to become very painful this led to further consultations until such time as a fasciotomy operation was arranged, the operation was carried out in July 2017.
Operation day
 I arrived at the Hospital at 7:30 am and was shown to the ward by the ward clerk. Within a very short time, I had been booked into the system had my blood pressure checked, and was ready for the day ahead. A short period of time later Mr Tollafield arrived and talked me through what he was going to do once I was in the operating theatre, then the anaesthetist arrived and checked all was well and that I had the obligatory thick black arrow on the right leg. By 9 am I was in the anaesthetic room of operating theatre 2 and waiting for surgery. Next thing I was in the recovery ward waking up to the dulcet tones of the recovery nurse Chris who proceeded to do all the necessary checks before I was returned to my bedroom on the ward. Mr Tollafield saw me after his operating list and said that he was very happy with the way the operation had gone and that I could go home and come back and see him in six weeks for a follow-up consultation.
I arrived at the Hospital at 7:30 am and was shown to the ward by the ward clerk. Within a very short time, I had been booked into the system had my blood pressure checked, and was ready for the day ahead. A short period of time later Mr Tollafield arrived and talked me through what he was going to do once I was in the operating theatre, then the anaesthetist arrived and checked all was well and that I had the obligatory thick black arrow on the right leg. By 9 am I was in the anaesthetic room of operating theatre 2 and waiting for surgery. Next thing I was in the recovery ward waking up to the dulcet tones of the recovery nurse Chris who proceeded to do all the necessary checks before I was returned to my bedroom on the ward. Mr Tollafield saw me after his operating list and said that he was very happy with the way the operation had gone and that I could go home and come back and see him in six weeks for a follow-up consultation.
Our technique is designed to start early ambulation 24 hours later and build up. Our physiotherapists take over the post-operative recovery and two small sutures are removed by our nurses. Unless problems arise we expect our patients to increase their activity and undertake the given stretches. Not all foot specialists are willing to use the MIS endoscopic technique, let alone the blind guide that I have used. The blade is protected by feeding a blunt instrument into the incision so it stays close to the fascial band.
“I wasn’t permitted to drive for 2 weeks after attending an outpatients clinic to have my dressings removed. Once home and after mastering walking with the aid of crutches I collapsed into my comfy side of the sofa and fell asleep. Later that first evening I found the anaesthetic was wearing off and the pain was starting to return along with a dull ache around my ankle, I decided to take 2 Ibuprofen tablets and go to bed to relax.”
Daily & Weekly diary after surgery
 DAY 2 After a fairly good night’s sleep I got out of bed and was pleasantly surprised to not have any pain only slight discomfort from where the incision was made. Next came the task of showering but with the aid of a fantastically simple device called a Limbo cover. This allowed me to confidently shower without getting my dressing at all wet, I continued to shuffle around that day but soon realised it was much easier to get about without the aid of the crutches. The next few days and over the weekend went along very pleasantly with no real pain to talk of just a little discomfort I did on occasion take the odd Ibuprofen just to keep things at ease.
DAY 2 After a fairly good night’s sleep I got out of bed and was pleasantly surprised to not have any pain only slight discomfort from where the incision was made. Next came the task of showering but with the aid of a fantastically simple device called a Limbo cover. This allowed me to confidently shower without getting my dressing at all wet, I continued to shuffle around that day but soon realised it was much easier to get about without the aid of the crutches. The next few days and over the weekend went along very pleasantly with no real pain to talk of just a little discomfort I did on occasion take the odd Ibuprofen just to keep things at ease.
DAY 6 I returned to the outpatient department at Little Aston Hospital to have my dressing changed and the stitches checked. This was the first time I’d seen the wound area and was pleased to see it wasn’t at all inflamed just a little bruised along the incision line, the nurse applied a fresh dressing and I was allowed home. Again there was no drama over the next few days then it was time to have the dressings removed for good.
WEEK 2 Back to the hospital this time to have my dressings removed and put my sock and shoe on also enabling me to drive once again.
WEEK 3 I’m finding that my ankle starts to ache by the end of the day so have taken to doing a little light stretching exercises before getting up out of the chair or sofa, also first thing in the morning before getting out of bed.
WEEK 6 Time for my post-operative consultation. After examining my foot Mr Tollafield was very pleased with the incision site and the range of movement. Because of concerns about the aching ankle he arranged a course of physiotherapy to exercise my foot and ankle with a much better-structured regime. I was then discharged from his care.
Conclusion
After continuing with the physiotherapy for 8 weeks I was told by the physio my state of health returned in both my feet and ankles although I found too much walking or being on my feet for long periods my right ankle and foot started to ache and I needed to rest for a short period then I can continue about my day. Life has returned to very near normal after a 7-year journey of living with the pain and discomfort of acute Plantar Fasciitis.
Reflection from John’s case
The majority of patients will benefit from surgery which should only be performed in recalcitrant cases. Of all the cases I managed, only one reoccurred after treatment. The benefit of surgery provides a quick and safe procedure where the post-operative scar is usually invisible to the naked eye. Lateral border foot aching can occur, but this arises because patients spend too much time supinating the foot, rather than a weakness arising from the surgery. This lateral instability for the most part is, therefore, a myth. Rapid recovery depends on the patient, their pain threshold, and willingness to work on the exercises. I always warn patients that this method, despite allowing fast mobility, still requires a 3-month recovery before all discomfort ebbs. The fascial band is thickest in the centre and many worry that a full band transection causes a problem. Tears within the FB that show up on ultrasound can benefit from the MIS surgical technique. Ali (2021) published results were undertaken as a clinical research paper and are worthwhile considering.
Results
At the end of the follow-up, the mean Americal Orthopaedic Foot Ankle Surgery (AOFAS) scoring changed significantly from 67 points before surgery to 93 points (P < .0001) which was clinically significant. Sixteen (53.3%) patients had excellent results, 8 (26.6%) patients had good results, 4 (13.33%) patients had acceptable results, and 2 (6.66%) patients had poor results. Three cases complained of postoperative superficial infection at the medial portal. Two cases developed numbness and paraesthesia at the sole of the foot. Three patients had ongoing start-up pain that resolved within two months. The mean duration to full weight-bearing after surgery was 40 days. All patients returned to full activities by a mean of 10 weeks.
![]()
Johannsen,F, Konradsen,L, Herzog,R, Rindom Krogsgaard,M Plantar fasciitis treated with endoscopic partial plantar fasciotomy—One-year clinical and ultrasonographic follow-up. 2019. The Foot. Volume 39
Ali, H. The results and safety of endoscopic plantar fascia release for the treatment of chronic plantar fasciitis. Journal of Arthroscopy and Joint Surgery. 2021.ISSN 2214-9635. https://doi.org/10.1016/j.jajs.2021.02.007.
Thanks for reading ‘Plantar Fasciitis and surgery’ by David R Tollafield
Sign-up for here my regular FREE newsfeed
Why not read Foot Health Myths Facts & Fables available from Amazon books
Published by Busypencilcase Communications Est. 2015 for ConsultingFootPain


Recent Comments