The bruised heel and common cause of heel pain
 If you have just selected this article, welcome. This article is only about bruised heels which form a common cause of heel pain. This is NOT about all of those types of heel pain you will find if you search the internet. The article does not talk, for instance, about fasciitis, spurs, heel pad atrophy, Baxter’s nerve, or tibial tendon dysfunction. This is specific to ONE condition only. That said, bruised heels form part of a range of conditions which are often called syndromes. By definition, syndromes are associated with a collection of signs and symptoms which can occur in combination. Therefore because this condition is an injury, and specific to one site, the heel pad, it is not a syndrome. It is often caused by a known injury. The impact of the heel hitting the ground with a repetitive force. This will be illustrated by my own case history. Cursory searches fail to identify this condition while other forms of heel pain are lumped together.
If you have just selected this article, welcome. This article is only about bruised heels which form a common cause of heel pain. This is NOT about all of those types of heel pain you will find if you search the internet. The article does not talk, for instance, about fasciitis, spurs, heel pad atrophy, Baxter’s nerve, or tibial tendon dysfunction. This is specific to ONE condition only. That said, bruised heels form part of a range of conditions which are often called syndromes. By definition, syndromes are associated with a collection of signs and symptoms which can occur in combination. Therefore because this condition is an injury, and specific to one site, the heel pad, it is not a syndrome. It is often caused by a known injury. The impact of the heel hitting the ground with a repetitive force. This will be illustrated by my own case history. Cursory searches fail to identify this condition while other forms of heel pain are lumped together.
A short link to Interpod is worthwhile a quick look.
The one most commonly described form of heel pain is fasciitis. Writing about unrelated foot conditions serves no purpose. The chances are, if you find an article about the heel pad, the subject is often about wasting of the fat pad. At the risk of being attacked by critics, the bruised heel pad is different to bone bruising. If pain fails to go away with treatment, then bone bruising is diagnosed by special scans known as an MRI. The link to the NHS shown, talks about other parts of the body and not the foot. The foot however is frequently scanned using this method. The use of a foam pad is discussed but you will realise that it is not the best answer.
Reading score = 72. Easy to read
My Patient Journey for managing the bruised heel
 This is a case history, or a feature that I call A Patient Journey. As a podiatrist I should know what I’m talking about. After 40 years I have treated many types of heel pain. If you want information about other heel conditions DO select one of my other articles. More Heel pain problems – pain series 4 is a useful place to seek out other information and remedies on this website.
This is a case history, or a feature that I call A Patient Journey. As a podiatrist I should know what I’m talking about. After 40 years I have treated many types of heel pain. If you want information about other heel conditions DO select one of my other articles. More Heel pain problems – pain series 4 is a useful place to seek out other information and remedies on this website.
Why did it happen?
 I was on a treadmill (shown), which is one of the most common exercise systems to be found in the fitness centre (gym). I was on a mission to loose weight, keep fit and tone up as well as ensure good cardiac stimulation. I was keeping a diary which I have recorded as my first gym diary series. Having already covered a month since gyms re-opened after Lockdown, I was now into my seventh week. Selecting goals was my new aim and the treadmill had a useful profile. This meant that the treadmill would automatically set a different speed every other minute. One minute I was walking, the next running and so on.The set speed took me from 5.6 Kph to 9.9 kph ever other minute.
I was on a treadmill (shown), which is one of the most common exercise systems to be found in the fitness centre (gym). I was on a mission to loose weight, keep fit and tone up as well as ensure good cardiac stimulation. I was keeping a diary which I have recorded as my first gym diary series. Having already covered a month since gyms re-opened after Lockdown, I was now into my seventh week. Selecting goals was my new aim and the treadmill had a useful profile. This meant that the treadmill would automatically set a different speed every other minute. One minute I was walking, the next running and so on.The set speed took me from 5.6 Kph to 9.9 kph ever other minute.
A deadly force to avoid
My heel starts to rise marginally at 7 kph. However, the heel does not fully leave the floor. To achieve little heel contact one would need to sprint, 100, 220 metres probably, which on the treadmill for most of us could be dangerous. To date I have run at 15 kph which is pretty fast for my age and the fact I also have a chronic knee problem. As the heel contacts the ground the impact forces vary. Heel pain was the result which came after my session.
The soft tissues (skin, fat, ligaments) are battered at this one point (see illustration below showing outside of heel contact point) for when I am walking slowly.
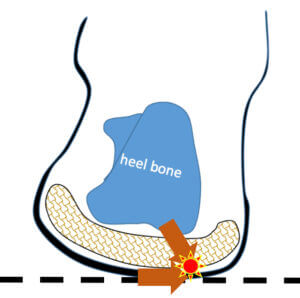
heel with diagrammatic impression of fat pad and combined direction of forces (C) 2020 Busypencilcase Reflective communications
The point of contact was the rear section of the heel pad. For the last 5+ weeks I had either walked or run, but not set the machine to alternate in such short bursts. The ‘profile’ programmed set this up. I was beginning to lament selecting this pre-set goal. Furthermore this was the first time I had set such a programme. Years ago I experienced this same pain on the treadmill but now I could be more objective about the whys. I was older by fifteen years, although my heel pad was still thick and viable. The skin was just a little harder than usual. There were no splits (fissures) which is a common condition often associated with heavy exercise, some shoe types and dry skin. I use creams on the foot to keep the skin (tissue) supple.
By the following Wednesday, 4 days later after the incident, I realised that I was not getting better and set about treatment.
How do you tell that you have a bruised heel pad?
Signs and Symptoms
The heel shows no signs of bruising, neither is it red or obviously swollen. The pain varies depending on the position of the foot . I could squeeze the heel pad and there was tenderness on the squeeze test but not when pressed underneath.The pain level was around 3-4 if my heel pad was squeezed hard from the side. Be aware, fasciitis presents differently.
. I could squeeze the heel pad and there was tenderness on the squeeze test but not when pressed underneath.The pain level was around 3-4 if my heel pad was squeezed hard from the side. Be aware, fasciitis presents differently.
Standing and remaining in one place caused more discomfort than moving around. Pain killers might dull the discomfort but they are not the answer. However, it does not harm to take an anti-inflammatory tablet at the acute stage. The symptoms include periodic pulsating discomfort. The heel does not like to be positioned with weight on the back of the heel, i.e driving.
I use my cruise control in the car as I use an ‘automatic’. This is helpful for a left foot injury. For a right foot you would need to use a cushioned heel guard (see below). If there had been a bruise around the heel then I would have considered bone or ligament damage. The level of pain can be described as 2-4, so more of a discomfort than real pain. To reach level 4 would arise after increased activity such as a walk. Then after rest this discomfort would ease. The early morning standing on the foot is different to fasciitis and does not appear as sharp or biting.
Mechanics
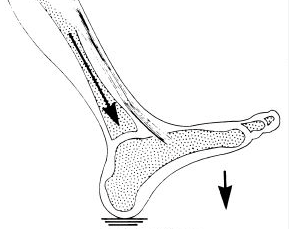
Heel contact and loading response.(From Perry J: Normal and pathologic gait, in Atlas of Orthotics, ed 2. St Louis, Mosby-Year Book, 1985, p 77.
To understand the mechanics of the injury we must appreciate that when contacting the ground, the skin and fat respond differently. The direction of contact is sideways rather than directly under the heel. This is why shoes wear on the outer edge and not the inner side normally. Several types of directional force are involved. One is called a lateral or sideways force, the other a vertical contact force. The foot has that peculiar feature in that it twists or rotates as well. Add lateral, vertical and rotationally twisting forces together and you have a group of forces that have collectively increased. The response to these forces acts differently within the deeper fat pad (illustrated above) and the skin.
The skin is more resistant and responds by thickening or forming a callus. This is normal. The fat pad however compresses, flattening then expanding. Because the skin is thickest on the foot the protection is excellent through its five layers of cells. Vertical forces alone are catered for well by the foot. However, the lateral forces do more damage. Such damage consists of tearing the connections between fat cells. These just happen to be rich in blood and the pad has inflammation and can swell. The more damage, the more swelling that arises following injury.
Related article
You can now read about the ‘gait cycle’ or mechanical components of walking under a new article called shin splints (Dec.2020). Shin splints can also arise in a gym as well as outside activities. Read here.
Why should one direction over another matter?
Scientists have found that some tissues like fat, deal with the stress of forces better in one direction than in another direction. This means the fat is stronger at vertical compression than lateral impact. The time factor, or length of contact makes a difference. The repetitious nature of stress can increase the damage in the material substance of the heel, the fat pad. The pad is made up of a matrix. Fat is surrounded by a fibrous patch network. The Tuli Heel pad (shown below) mimics this and is the reason this particular design is better than a piece of foam. Many off the shelf foam pads help a bit but do not help a lot.
The dangers of short intervals
The short periods of exercise seemed to create more heel pad stress at one-minute intervals. The idea was to test this theory out by lengthening the intervals and developing a different strategy. I also needed to stabilise my left foot in particular and so I added a prescription orthotic to my running shoe.
If a foot overpronates, which means it leans in, the excess movement can add to the strain and even cause plantar fasciitis. The period when the foot is less stable is when the heel strikes the floor and the weight moves onto the front of the foot (forefoot and toes). This takes but part of a second to occur, but it is sufficient to make the fat pad tear internally. These tears are small or micro-tears but they do cause inflammation and increase fluid release. Repair starts rapidly but because the heel is used frequently, any resolution takes time. My last event took 2 weeks to settle and so I would expect a similar recovery period.
Fast forward to WEEK 4
At three weeks the heel pain had eased. I had a week off but went walking using my Tuli heel cup. This meant I could keep going as long as the discomfort was contained. Back at the gym now I decided to go for the treadmill at the start of week 4 but would make sure that my heel would mainly be set in the running mode – 7-10 kph.

orthotic typically has a contoured heel and may finish before the toes or be produced with the full length of the foot
I used my prescription 3/4 length orthotics which fall behind the ball of the foot (outline illustrated). I did 21 minutes and started with a gentle 5 Kph then built it to 9 kph. The difference was that by using longer periods in between the shock of the heel hitting was less. I had learned my lesson from the short intervals. This meant my tissues could recover. I, therefore, discovered the secret was about the time allowed for tissue recovery. One minute between impact speeds meant it was poor.
Three minutes at the slow speed to warm up then 10 minutes at the faster speed. I dropped it to 3.5kph for some rest. I checked the heart rate and waited for this to come down to around 115 beats per minute. The machine enables all of the information to be viewed. I then set the gradient to its maximum pitch of 15%. The speed went back up to 5 kph for another 5 minutes and then dropped for a short rest at 3.5kph and then onto 10 kph for the remainder of the time. I was even able to do my fast burst of 13-15kph and ill effect.
Self help strategy


Tuli Heel cup available for around £8-10 (pair)
We want to avoid drugs. Using anti-inflammatories for a few days won’t hurt e.g. ibuprofen. I made a soft heel pad out of foam and ordered a special heel cup called a Tuli heel (shown). I dug out my custom orthotics because I had not used them for a while. I had also noted some tendon discomfort and now this ensured I would take all precautions to reduce the shock. The orthoses (orthotic) would stop over pronation and control my foot when walking.
Despite using a foam pad, the heel cup and orthoses, I found a three-day rest from the gym helpful. But this did not resolve the heel immediately. I cut back on walking and noted burning discomfort for around 10 days.
Patience is important
I used some voltoral gel and movelat. Neither was particularly helpful but using a basic foot cream was useful to keep the skin supple so this could support recovery. Deep massage for 2-3 minutes worked well.
The foam adhesive pad was useful but did not help as much as the Tuli Heel. Sitting, which I do a good deal of when writing, was variable, but moving around helped more. The heel pain on day 8 was controlled but I still had symptoms. Having cut out all of the treadmill work I used the cross-trainer using my heel cup daily and orthotics in the gym.
So lessons learned? YES
- We can treat the heel provided that we identify early on the reason for the problem. We have to stop the primary activity but ideally keep mobile.
- Total rest is not ideal for heel pain unless of course there are medical complications like fractures or infection. Rest actually means reducing the activity.
- Skincare is important as well as using some heel pad containment systems. The Tuli Heel Pad worked well initially. A foam heel pad, being flat, may cushion the heel, but the benefit is limited.
- Bruising takes THREE WEEKS to settle, less maybe with the withdrawal of overactivity. I continued to trek walk during my recovery and so will have perhaps slowed matters. However, I was only experiencing low pain grades of 2-3 mostly.
- The use of a good heel cup and contoured orthotic worked last time and did again.
- Adjust your programme whatever. If you are at a gym look to those profiles, or pre-programme features. Although intended to help you keep fit, they can add an unsuspected injury to your life.
- My intervention, skincare, containment, change of activity and altered programme worked. I am delighted to say today at the end of week 4 after first experiencing pain, I am now back to full running on the treadmill.
What if it doesn’t help?
Of course, everyone is different. If your pain persists then cut back activity further. You can ice your heel but then that suggests your inflammation is growing. Check your heel cord is not too tight and exercise this a little. The information contained in this NHS information piece may be useful.
Some benefits will be achieved with anti-inflammatory gels but alone this does not work. If by 5 weeks there is no improvement then seek professional advice otherwise persevere with the conservative methods.
Thanks for reading – ‘Heel Pain due to a bruised heel’ by David R Tollafield
You can now read Foot Health Myths Facts & Fables by David R Tollafield published on Amazon books
Sign-up for here my regular FREE newsfeed
Published by Busypencilcase Communications. Est. 2015 for ConsultingFootPain



Thank you! After hours of scrolling through the internet, I finally understand what my heel pain is and how best to treat it. I have ordered the heel cups, but need to investigate further the best orthotics for my biomechanics.
I have seen that taping is beneficial in the recovery period, so will also try that.
As a fanatical runner, I need to do everything possible in an attempt to get back out there!
Thanks again for such a precise and informative post. CFP response: thanks Kate I am pleased to hear that the information has provided some value. Please tell your friends and if there other questions please write. My contact information is on the home page.
Hi and thanks for the article! This might be what I have right now in both my feet/heels. I’ve read alot about fat pad syndrome and plantar fasciitis but none of them exactly fits the bill. Especially the part where you mentioned that you could press pretty hard right under the heel without feeling any pain is similar to what i experience. Also i don’t have any sharp pain during mornings or anything like that. It’s an aching dull feeling and i wouldn’t exactly call it painful. If I have to put a finger on where I feel it the most it has to be on calcaneus bone just at the back of the heel, the rounded part where it stops being the “leg” and starts being the foot, just in the middle of that (sorry I’m not a native English speaking person). Where i press that spot i can sometimes be painful but not alot. Was it the same for you? I couldn’t really tell from the text. CFP response: An idea Henrik why don’t you send me a picture of your foot marked where you find it hurts. I think this would be more helpful and I can respond. A side view and back view in good light make for easier observation. Please use busypencilcasecfp@gmail.com
Henrik,
Your explanation is fabulous and exactly where I feel it. It’s the calcaneus bone (at the side) and the tendons nearby are also tender.
I have now rested for 2 weeks and am thinking about attempting a run tomorrow, but I’m nervous in case I inflame it all again. I really don’t want to go back to the start again!
I have had some acupuncture and that seemed to help. Additionally, I have realised that icing it is actually accentuating the pain now and not assisting it.
Henrik, fingers crossed we get a similar result to the original article and that it starts improving in the next couple of weeks.