Diabetes and the foot
A quick refresher
Diabetes and the foot is the staple diet of podiatric medical management. It should be remembered that diabetes is a disease where the body has a poor ability managing sugar digestion. Insufficient production of insulin in the pancreas affects many parts of the body at a cellular level.
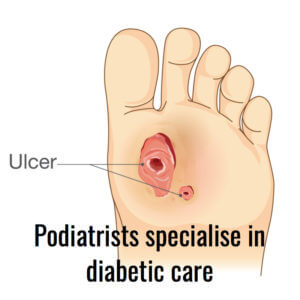
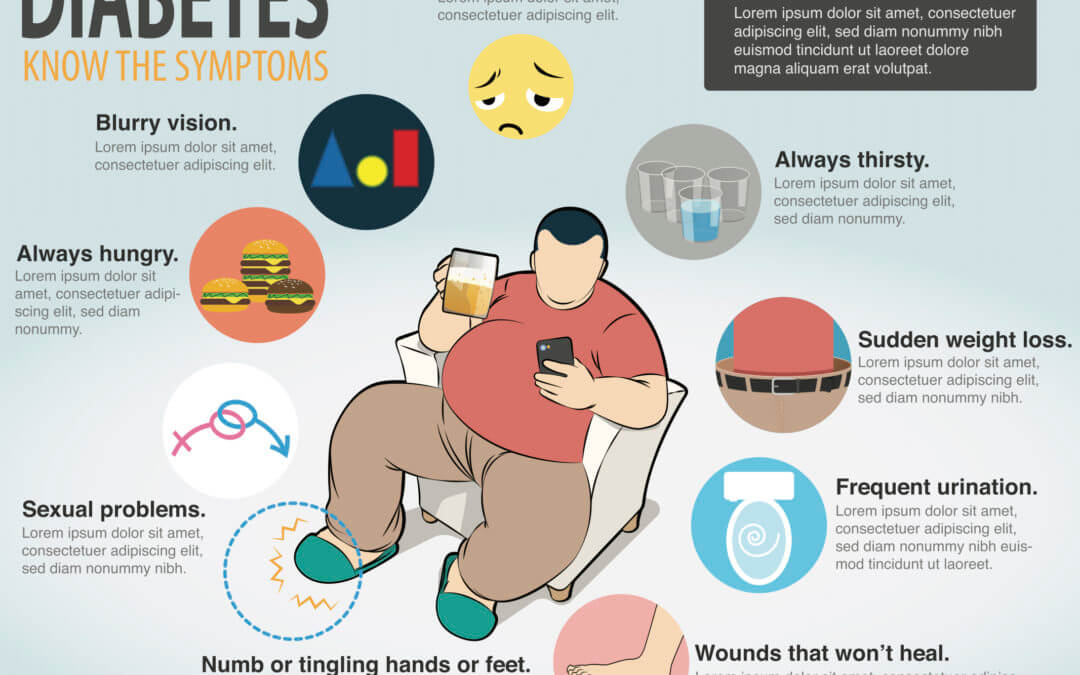
The key effects however lie with blood vessel disease and damage to nerve pathways. The organs most affected, if untreated, include the kidneys, eyes, skin and heart. Anything that relies on a good working flow of blood can also be affected and so the feet are at greater risk from poor healing and cannot feel sensations such as sharpness. Failure to recognise damage under the foot can lead to wounds that cannot be felt in the usual way. An undetected wound deteriorates faster than in patients without the disease. Infection arises because of poor circulation, poor tissue quality and the numbness that may become more profound. Ulcer formation is not unusual and these can become deep or perforating through layers of skin down to joints.
 As the disease progresses organ damage is evident elsewhere. In modern society we now recognise that diabetes can lie alongside other conditions including thyroid problems, rheumatoid arthritis to mention but a couple.
As the disease progresses organ damage is evident elsewhere. In modern society we now recognise that diabetes can lie alongside other conditions including thyroid problems, rheumatoid arthritis to mention but a couple.
The aims from early podiatric intervention ideally will help reduce the risk of ulceration, infection and amputation. Some 5% of patients die following amputations to legs following diabetic complications.
Serious risks: heart attack, stroke, loss of limbs, infection, blindness, kidney disease, damaged nerve system
What can podiatrists do for diabetics?
 The three main contributions podiatrists make are to diagnosis the condition, to monitor the disease together with local GP practices, and to manage skin and foot infection. Managing skin damage includes reducing any damaging pressure load on the foot. This has now become a sub-specialty within podiatry.
The three main contributions podiatrists make are to diagnosis the condition, to monitor the disease together with local GP practices, and to manage skin and foot infection. Managing skin damage includes reducing any damaging pressure load on the foot. This has now become a sub-specialty within podiatry.
DIAGNOSIS
Diagnosis of diabetes is often identified in the urine. Protein, sugar and blood feature as abnormal constituents as well as urine pH and presence of white blood cells.
Clinically we look for loss of weight, loss of energy, water work infections, skin infections and delayed healing, especially in the foot. Eye problems and kidney problems don’t start as soon as other signs but nonetheless provide indicators of the condition. Loss of libido (sex drive and desire), especially in men. Together with an increased thirst there may be an increased need to use the toilet.
MONITOR
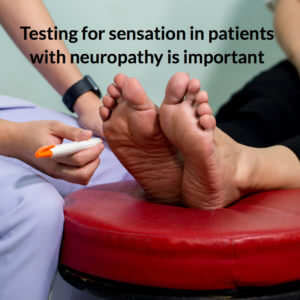 As the NHS focuses more on risk, resources are distributed to clinics specialising in diabetic foot care. The monitoring phases falls to all trained podiatrists who can undertake tests for peripheral neuropathy, and early sign that the disease is NOT STABLE. Skin sensation includes both sensory assessment for vibration, sharpness, light touch and temperature changes. Muscle power can be lost and reflexes can be tested.
As the NHS focuses more on risk, resources are distributed to clinics specialising in diabetic foot care. The monitoring phases falls to all trained podiatrists who can undertake tests for peripheral neuropathy, and early sign that the disease is NOT STABLE. Skin sensation includes both sensory assessment for vibration, sharpness, light touch and temperature changes. Muscle power can be lost and reflexes can be tested.
Pulses can be palpated and audible flow checker with clinical machines called Doppler ultrasound. This also allows the podiatrist to listen for unusual heart sounds, signalling conditions such as tachycardia and atrial fibrillation, to name but two. Blood pressure can be checked to see the effect of blood flow through the heart. Tests for quality of flow to the limb are also carried out. Don’t be surprised if your arm and ankle are measured to determine the relative quality of flow. Patients should always report calf pain on walking short distances as this could be related to blood flow (vascular disease). Some machines can measure oxygen flow.
All diabetics are at risk from different disease levels broken into Types I and II, dietary, tablet and injectable controls. Podiatrists can help with smoking and can refer to teams for smoking cessation after analysing urine or breathing for carbon monoxide. Podiatrists are trained in medicine and physiology as well as pharmacology and so have an appreciation of overall health.
 Blood testings can look at the level of sugar (glucose) in the blood or we can test the uptake of glucose within the haemoglobin often called glycosylated haemoglobin or HbA1c test. A standard blood test may be less reliable than a fasting test where no food is taken initially, or the blood can be loaded with sugar and the level of sugar monitored based on how fast the insulin regulates it. The pin prick test is carried out by thousands of patients each day using a glucometer. This provides an immediate cost effective test for the patient so they know how well they are doing.
Blood testings can look at the level of sugar (glucose) in the blood or we can test the uptake of glucose within the haemoglobin often called glycosylated haemoglobin or HbA1c test. A standard blood test may be less reliable than a fasting test where no food is taken initially, or the blood can be loaded with sugar and the level of sugar monitored based on how fast the insulin regulates it. The pin prick test is carried out by thousands of patients each day using a glucometer. This provides an immediate cost effective test for the patient so they know how well they are doing.
MANAGEMENT
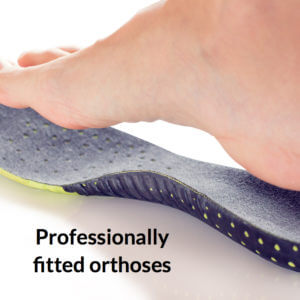
Tissue that is most susceptible arises from the skin and nails but these are not the only tissues involved. Muscle weakness and joints can develop problems if the condition is not checked over time. Ulcers penetrate (perforate) down into the deeper layers if untreated and patients do not take the condition seriously. Podiatrists aim to heal the skin, deal with infection using dressings, local medication and antibiotics. Taking pressure off the skin is vital to allow skin to heal but today many new dressings and materials offer assistance to both podiatrist.
Orthotic management can make a major difference to foot stability. All of this takes time and many months and hundred of pounds can be spent by the NHS managing ulcers to prevent amputations.
 The role of managing diabetic care is attractive to many podiatrists who desire to increase their expertise and improve their career. As diabetes is one of the key risks, but not the only lower limb risk, podiatrists will have been qualified a number of years before running these clinics, often alongside consultant diabetologists.
The role of managing diabetic care is attractive to many podiatrists who desire to increase their expertise and improve their career. As diabetes is one of the key risks, but not the only lower limb risk, podiatrists will have been qualified a number of years before running these clinics, often alongside consultant diabetologists.
SURGERY
Surgical intervention is often needed to deal with skin gone bad (necrosis). However patients need to be better medicated and stable before surgery is wise. Vascular surgeons remove legs when the foot becomes gangrenous and the podiatric surgeon today is extending his and her skills into dealing with diseased joints (neuropathic arthropathy) as well as limbs. Revascularisation is risky and not performed if good blood supply is unavailable. Limb amputation is the end game but carries risk of early death for some. Minor amputations of digits may be carried out to avoid risk of tissue death deteriorating but the surgeon has to removal all tissue until fresh available blood supply can be find.
Taking the disease seriously
The biggest problem is that many diabetics, after years see themselves as normal, try to live as such, often at the expense of sliding back into unstable disease. Obesity does not help, neither does poor fats in the body which clog arteries. Alcohol and smoking are poor allies of diabetic disease.Keeping the sugar (glucose) balanced with insulin is important. The aim of medicine is to reduce the strain on the pancreas and its insulin producing cells. Society does not need additional salt and sugar in our food but until we realise this the fight against obesity, high blood pressure and high cholesterol will continue provoking late onset (Type II) to arrive. When this is seen in young adults there is a real worry that life expectancy shortens and the cost to the health economy rises. Modern drugs and indwelling slow release systems aid the diabetic live a normal life as possible. Early diabetes Type II is reversible compared to Type I, where people are born with the generic effect.
Thanks for reading ‘Diabetes and the Foot’ by David R Tollafield

Busypencilcase Reflective Communications Est 2015
29 April 2020


Recent Comments