Behind the scenes stories
 This series covers stiff toe surgery and different patient stories taken from their own words. All had stiff big toe joint pain, and some had bunions. Surgery was successful in the main, but as shown, there are no guarantees. What do you need to know when things don’t go according to plan? Blue highlights will take you to different links and help build a picture depending on the detail you need. My clinician’s comment will elaborate on the storyline and provide further information. Please read the other cases on ConsultingFootPain. Each story will paint a different picture. Launching 1st July 2021 and on successive days this week.
This series covers stiff toe surgery and different patient stories taken from their own words. All had stiff big toe joint pain, and some had bunions. Surgery was successful in the main, but as shown, there are no guarantees. What do you need to know when things don’t go according to plan? Blue highlights will take you to different links and help build a picture depending on the detail you need. My clinician’s comment will elaborate on the storyline and provide further information. Please read the other cases on ConsultingFootPain. Each story will paint a different picture. Launching 1st July 2021 and on successive days this week.
Please note that the techniques described and advice will vary between surgeons and centres. The variety of options on the market is extensive. This author only describes techniques patients have reported concerning their stiff toe stories.
Read each patient’s story covering the stiff toe:
Leah- both feet fusion surgery (arthrodesis)
Tom – fusion surgery after an implant
Rachel – both feet – implant surgery after an osteotomy
The patient tells their story
Nothing resonates better than a patient telling their own story. We learn more from an undiluted tale than one which is sanitized. I felt strongly about writing and publishing a book about bunion and bunion surgery. It is a fact that at most conferences I have attended, clinicians speak about successes, not their problem cases. I am keen to raise awareness because we learn from problems and how to solve them. I had back surgery twice. The second was a revision. It is a fact that surgery does not always work, and revision is necessary. With litigation at an all-time high, the more laypeople understand why things don’t work may alleviate much of the grief that follows unsuccessful results. I call this ‘behind the scenes’ because some conversations are unclear. It is worth reading Tom. Tom was not a patient of mine, and his case developed from an interview in 2019.

ConsultingFootPain (CFP) has already published advice on bunions and some information about the joint stiff toe. Protecting the skin and reducing pain can be achieved, but there comes a time when surgery is required. Leah had both her big toes operated on to fix her pain. Tom and Rachel needed revision surgery. I will follow these patients as they record their own stories. I started interviewing and gathering their initial journey notes and charted their progress. All may not appear as it should be. Three different orthopaedic and podiatric surgeons operated on each patient. It is not the purpose to advise which surgeon to seek but clearly, surgeons who are dedicated to operate on feet should be chosen over general surgeons. Not all orthopaedic surgeons specialise in feet, while podiatric surgeons do. I will use more information to describe the various techniques later in this article using selected video films.
Why do stiff toes develop?

stiff toes may be predictable with bumps
Damage to joints involves the cartilage (arthrosis), the joint lining (synovitis) and a bony bar formation (osteophytes). These are the bumps (shown) and ridges. Once the toe distorts and mishaps, shoewear comfort is reduced with increased skin pressure. Corns form, and in the winter, chilblain threatens to ulcerate. For many, the way forward is to select surgery. Foot surgeons, that is, orthopaedic and podiatric surgeons, will try to preserve the joint. Injections in joint spaces are performed under X-ray or ultrasound imaging. As the joint stiffens, the space between the two bone ends makes introducing any substance nearly impossible. Getting the injection into the joint is one problem, but lack of movement means the substance fails to move around the lining. The result is a failure. The joint is usually x-rayed before an intended injection treatment.
Some may use different methods like ultrasound and bone scans. Over 70% of bunions (hallux valgus) have some cartilage damage.

Spasm leading to pain and stiffness
If the joint is stiff but tightly bound because of spasms from smaller muscles, this part of the problem could be helped with an injection of anaesthetic and steroids. This condition is often associated with the sesamoid. The sesamoid is a small bone under the first metatarsal head.
What operations can a surgeon use?
There are three primary operations and a straightforward surgery. Simple surgery means that little more than the bone is trimmed flat, called an exostectomy or cheilectomy. Both work the same way. Pain may be relieved, but stiffness can result, which does not matter if the pain has disappeared.
Does the cheilectomy work?
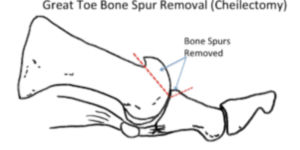 Bone shaving surgery reduces pressure around the joint so the skin can recover, and shoes may fit better. However, it does nothing for cartilage damage and can increase painful movement. My tip is to try protecting the foot first with cushioning sleeves and covers or change any tight-fitting shoes. Many cheilectomies are performed for their perceived simplicity, and most foot surgeons will attest to failures and revisions! Today’s three main operations include opening the joint to give it a bigger gap (osteotomy). The joint can be made permanently stiff (arthrodesis), and lastly, the joint can be replaced with a new surface (prosthetic replacement).
Bone shaving surgery reduces pressure around the joint so the skin can recover, and shoes may fit better. However, it does nothing for cartilage damage and can increase painful movement. My tip is to try protecting the foot first with cushioning sleeves and covers or change any tight-fitting shoes. Many cheilectomies are performed for their perceived simplicity, and most foot surgeons will attest to failures and revisions! Today’s three main operations include opening the joint to give it a bigger gap (osteotomy). The joint can be made permanently stiff (arthrodesis), and lastly, the joint can be replaced with a new surface (prosthetic replacement).
All foot surgeons learn about different techniques but will develop their preferred procedures over time. In each case described in this series, the right decisions were made.
The arthrodesis
 Leah had an arthrodesis, which means cartilage was removed from the ends of each bone making up the joint, and the two ends pushed together, then fixed as if the bone had been broken. End-to-end bone knits well and becomes solid without affecting the walk-on. The key point to be aware of is that patients who kneel for their occupation can also not perform. Sometimes the metal fixation, shown as a plate, may need to be removed later. This does not affect the result unless the bone bonding fails.
Leah had an arthrodesis, which means cartilage was removed from the ends of each bone making up the joint, and the two ends pushed together, then fixed as if the bone had been broken. End-to-end bone knits well and becomes solid without affecting the walk-on. The key point to be aware of is that patients who kneel for their occupation can also not perform. Sometimes the metal fixation, shown as a plate, may need to be removed later. This does not affect the result unless the bone bonding fails.
Osteotomy
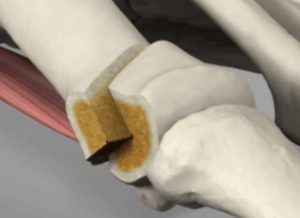 Rachel had an osteotomy. Osteotomies are cuts made in different parts of the bone and then allowed to heal like a fracture. It is a procedure that does not damage the joint directly but moves the bone in such a way as to create a gap so the joint can recover movement. The cartilage is preserved. Osteotomies [Video] need to be fixed with a screw(s) and sometimes plates which have been described in two of our patient stories. This type of fixation allows early mobility. The illustration shows one of the more straightforward techniques called a Chevron osteotomy. This is depicted in the short animated film 1′ 30” long and has no gory sights.
Rachel had an osteotomy. Osteotomies are cuts made in different parts of the bone and then allowed to heal like a fracture. It is a procedure that does not damage the joint directly but moves the bone in such a way as to create a gap so the joint can recover movement. The cartilage is preserved. Osteotomies [Video] need to be fixed with a screw(s) and sometimes plates which have been described in two of our patient stories. This type of fixation allows early mobility. The illustration shows one of the more straightforward techniques called a Chevron osteotomy. This is depicted in the short animated film 1′ 30” long and has no gory sights.
Prosthetic Replacement
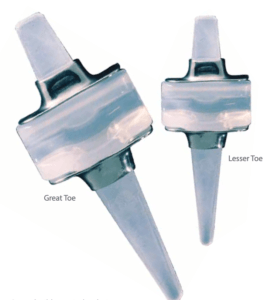
Swanson implant (silicone) C/O Wright Medical
A new joint surface spacer was given to Tom and Rachel, where the cartilage was heavily damaged. The spacer was made from medical-grade silicone (illustrated). A standard information sheet from Hereford Podiatry (NSH) is available. Joints can be made from other materials, including high-density plastic, metal and less popular ceramic materials. A cap or plug can be inserted into defective cartilage areas to resurface the joint. This technique is gaining popularity. Another replacement technique includes grafting cartilage into different sites to generate average cartilage growth. This has been popular in knee arthrosis and continues to develop.

Many films can be found on YouTube. Some are out of focus, too long and in many, the language may be too complex for most people to understand. In this video, U.S podiatrist Jennifer Boeri from the Holy Cross Institute has put a 5’35” video film together explaining the complexities of the rigid toe problem. The film covers many options for those wishing for more information.
What was the outcome?
What could go wrong, and what would our patients need to know before agreeing to perform surgery? Did surgery work out for all of them, and if not, what happened? Please read further to learn more… You can also read my bunion operation advice sheet – the big five.
Thanks for reading ‘Painful Stiff Toes and Patient Stories’ by David R Tollafield
A Behind the Scenes Patient Journey Series
Why not read more about the bunion (Hallux Valgus) behind the scenes on this website or buy the e-book/paperback by the same author?
David is an author and retired podiatric foot surgeon
Published by Busypencilcase Reflective Communications Est. 2015
2nd July 2021. Modified August 2024.


Recent Comments