Can we treat our own corns? Part 1
Have you ever used a corn plaster or similar to treat a corn on your foot? For many, a corn is seen as an inconvenience that can be pared down at home or treated with a corn plaster, available from a pharmacist. This article goes deeper into the subject for those with an inquiring mind. In Part 1 I explain the corn and why it is resistant to treatment.
Kilmartin (2016) writes a pithy yet all too true headline in his paper with Lopez and says, “Could it be that a sharp knife and a bright light are no longer enough?” Doubtless, scalpel skills are an exceedingly prized skill that do not arrive overnight, but the point here is that removing a corn is a temporary measure when used alone.

What and why?
We must understand what a corn is, why it forms and why treatments do not come as a package as we would find with infection = antiseptics or antibiotics. To understand this scene better, we need to look at the evidence from recent literature. Could an antibiotic be of value, or should we inject the corn with silicone or use a plant’s chemicals containing podophyllin? We might even consider cutting the corn out – but will it come back?
What is a corn?
We cannot assume a corn and callus are the same things. We know the two co-exist in many, but not all, cases often referred to as hyperkeratoses. The skin has a series of complex layers of cells called strata (stratum). The top layer is called the epidermis, capped with a waxy structure made of a protein – keratin (see illustration Farage et al. 2007). Between the epidermis and dermis, a defined layer called the basement membrane separates the epidermis and dermis and yet is intimately joined by cellular changes and processes allowing repair, fighting infection and regeneration. The skin has many specialised cells, including those with a pigment called melanin.
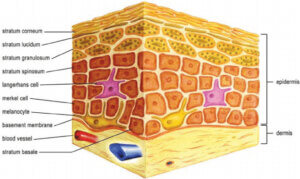
Normal skin structure (Farage 2007)
The corn is part of the keratin layer and does not penetrate the basement membrane because the area would bleed if it did. There are other reasons the dermis is penetrated, not least due to penetrating splinters. However, in some cases, infections and changes arise where blood vessels become invested between the dermis and epidermis, as seen in wart infections (a virus). These have been erroneously called vascular corns or neuro-vascular corns. Histology has been performed on many patients (author), with all excised tissue sent for analysis. There has not been one case where the changes cannot be explained or associated with a defined pathology. However, many samples are returned as ‘corns’ or keratin without defined fibrous or nerve-invested corns. Some tissue does involve nerves, but this emanates from deeper in the tissue. Painful corns have been associated with nerve pain, yet current evidence shows the pain is associated with a viral infection or deeper scar tissue from a previous injury.
If infection from a fungus, virus, or foreign body is involved with the skin, then pressure does not play as much as a reactive basal layer, causing further corn and callus formation without pressure. This means the infection can induce greater cellular activity. Lopez (2016) worked with Kilmartin to produce one of the few histological papers findings after full surgical removal corns had a 51% incidence of viral infection with the human papillomavirus (wart). They fully excised corns from forty-three patients.
If a corn was allowed to grow without pressure under the sole, it would form a horn as it is part callus (cutaneous horn). This is an oversimplification as pressure and skin stress cause callus in the first place, and so, in theory, you would still require pressure of some kind to stimulate new growth.
For some time, podiatrists have believed smoking caused such lesions. While the latter implication has not been substantiated, much evidence supports skin changes arising due to the effects of smoking. Lopez identified thirty-three patients out of forty-three (77%) who smoked of which many did less well from surgical excision.
The discomfort level is heightened if pressure arises with an infected corn. Bacteria can become involved, but pus forms more often due to a build-up of pressure under the skin, and turns out to be sterile rather than infected. The use of agents such as salicylic acid, commonly found in corn plasters sold online and from pharmacists, can cause secondary bacterial infection, and this point is inferred in the NHS link above.
Defining a corn
Lee, a dermatologist from South Korea, provides a useful definition (2014). The primary source, Dockery 1997 – A corn is a hyperkeratotic lesion with a central conical core of keratin that causes pain and inflammation. Some will divide a corn into hard corn or soft corn. The only difference lies in the amount of tissue moisture within the surrounding area and for this reason, soft corns are found between toes where sweat can build.
The cause of corns arises from chronic pressure and skin irritation from poorly fitting shoes. An intractable keratoma is a corn that resists treatment and can affect a patient’s quality of life as the condition worsens. Debridement is advised under a local anaesthetic if not tolerated, and there are plenty of reports where this has been carried out without such support. Imagine having dental treatment today without pain relief. All podiatrists are qualified to use local anaesthetics.
Podiatrists and Foot Health Practitioners offer management of corns and callus as part of overall foot health management. Scalpel debridement reduces the overlying top layer of the callus, and the conical component is enucleated. The common sites are the sole, forefoot mainly but also the heel. Other sites include the end of digits, overlying the knuckle part of the digit and in between and on the inside of toes. Where the foot has hard prominences such as bunions and heel bumps, calluses and corns can form, heightening the argument that pressure is responsible for such formation.
The peculiar conical shape has never been explained, although deep ridges of callus can be found in some feet emulating corn formation. The conical forms are, without a doubt, more painful. After professional reduction and enucleation, something the corn plaster does not achieve, a white dense line is visible to the eye – see the featured image at the top of this article.
Since the time that Durlacher described corns, this has been viewed as fibrous in nature and suggests a capsule separating the corn from the adjacent skin structures. Histology, that is to say, skin samples that include full-depth removal below this layer do not reveal scar tissue or fibrous organisation to support what has been a theory postulated in 1845 and repeated like Chinese whispers ever since. Once podiatry established a surgical sub-speciality, the podiatric surgeons started to examine the skin and the reports coming back from the histology laboratory, and the true nature of corns became more apparent.
The skin is exposed to pressure which, in mechanical terms, we understand as forces loaded upon an elastic structure. The skin has a firm matrix of collagen and elastin fibres within the lower layer of tissue called the hypodermis. We can call this fat. There are different fat cells in the body. Still, this fat is part of the anatomical system that protects nerves, affords a matrix for blood vessels, and provides insulation and cushioning. It is the latter function we are drawn to regarding the foot. Fat provides a soft impact. The tissues, skin, dermis and hypodermis each have unique mechanical stress properties. Compression and shear cause deformation with pressure, followed by recovery. Corns often form at the edges or between the ends of the long hard bones called metatarsals. The ends are often known as the ball of the foot. Although a corn can be removed and offer comfort, the lesion can return if the forces are not alleviated or altered. If the fat is damaged, the blood supply is altered, or if there is an infection or foreign body (hair, splinter), the corn will not respond to treatment.
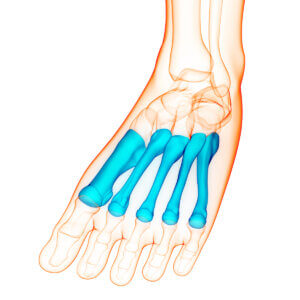
metatarsals with enlarged heads forming the ball of the foot
Toes in general
The first part of management is to check the inside of the shoes. If the toes are hammered, the knuckle sticks up, forming a callus and corn; the shoe should be carefully selected to reduce this risk. Older shoes have linings that can tear and irritate the skin. Remove all old damaged shoes from your collection. The toe box needs to be soft and deep. Use silicone or gel covers for toes to help protect them. Reducing the bulk of skin is best left to a professional to ensure the skin is managed carefully. Toes respond excellently to surgery where the whole lesion is removed and the toe position corrected.

Pre-corn showing skin thickening with a callus. There is no nucleus but note the knuckle is inflamed and swollen, suggesting deeper tissue involvement. This problem can be protected with careful shoe choice initially
The forefoot and sole
If space allows in the shoe, sometimes a soft inlay or insole is beneficial, especially if the fat pad is thin and the skin appears thin and tender to the touch. You can reduce callus with pumice stones and similar abrasives, including the newer rollers. These rollers will not remove corns that are well established. The basic atlas covering skin lesions under the forefoot can be downloaded here – https://consultingfootpain.co.uk/wp-content/uploads/2022/10/ATLAS-2.pdf
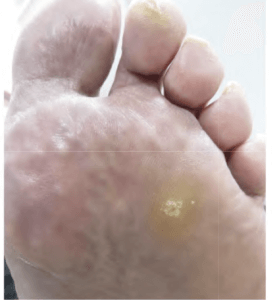
Corn before debridement between the 3-4th metatarsal
The foot heel can be exposed to unpleasant corns causing considerable pain, limping and disability. Heels are renowned for being infected with the wart virus. A deep aching sense and tenderness on pressure indicate a careful skin examination. A form of corn called seed corn exists in lax skin often found in the long arch of the foot. Smaller than many corns, these can be managed with softening creams to keep the foot hydrated.
Interestingly, warts are often thought to affect children who visit public swimming baths, and in adulthood, this infection seems less prevalent. However, we know from biopsy and skin excision that older patients harbour these infections within corns in as many as 50% of cases (Lopez, 2016). As we age, skin alters, and resilience diminishes with shoe pressure and activity, (Farage et al. 2007). In the next section, I look at the corn plaster using salicylic acid and consider other chemicals used during the last two decades. In Part 2, I look at some treatments, including corn plasters and podiatrist treatments.
![]()
- Farage, Miranda et al. from Cutaneous and ocular toxicology. Structural Characteristics of the Aging Skin: A Review. DO – 10.1080/15569520701622951
- Lee, W.J., Lee, S.M., Won, C.H., Chang, S.E., Lee, M.W., Choi, J.H. and Moon, K.C. (2014), Efficacy of intralesional bleomycin for the treatment of plantar hard corns. Int J Dermatol, 53: e572-e577. https://doi-org.libaccess.hud.ac.uk/10.1111/ijd.12586
- Lopez, FM Kilmartin TE Corn Cutting in the 21st Century. Podiatry Now. October. 2016
- Tollafield DR Musings about corns and callus. May 2022. ConsultingFootPain
- Tollafield DR Obstinate Corns over Tendons October 2022. ConsultingFootPain
- Tollafield DR Hard skin on our Feet. November 2022. ConsultingFootPain
Thanks for reading ‘Treating Corns on Feet – Part 1’ by David R Tollafield
Published by Busypencilcase Communications. Est. 2015

David is the author-editor of ConsultingFootPain (CFP) and a former podiatric surgeon. Articles are published each month on this site. Sign up for his newsfeed

Recent Comments