That Painful Foot Nerve
Medicine is curious. Most findings are accidental, names are confused, and it takes decades to refine the truth behind the first observations. In this hopefully easy-to-read article, I have offered some background research for my lectures and book. Here is a pain that Filipio, Lewis, and Thomas discovered in the 19th century.
The backdrop to our story
Consider the anatomist in Italy in 1835 looking at the foot while his somewhat deceased patient allowed him some anatomical exposure. Out pops a neuralgic ganglion, so he says it in his later published works. This was more curious as Filipio Civinini was a cranial anatomist. By the next decade (1846), a podiatrist had identified and written about a rare but interesting pain between the second and third toes in a few patients in his treatise. Lewis Durlacher, known as a surgeon chiropodist had treated William IV and allegedly Queen Victoria.
Moving from Europe to the USA, Thomas George Morton claimed the prize, and his name was stuck. First, he was a published surgeon in a medical journal, and second, his observations were much more open than Durlacher’s. However, Morton 1876 published his paper and talked about the fourth toe joint – the metatarsophalangeal joint. Being used to amputation surgery in the American Civil War (1861-65), he executed cutting out the joint rather than the nerve alone.
Morton’s plantar digital neuroma
A man named Hoadley removed the nerve around 1893. Much less famous than Morton, he set a trend for managing this curious but rare foot problem. Indeed, it is rare, at 88 per 100,000 in females and 50 per 100,000 in males, according to data taken from a large database by Latinovic (2006). Morton’s neuroma, also called a plantar digital neuroma (PDN), is far more common than Durlacher’s second-third toe neuroma.
Anatomical variation
There are two reasons for it being painful around the 3rd and 4th toes. A branch between two nerves can become compressed (Diagram Govsa). That compression affects the blood supply to the nerve, and the nerve swells, becomes inflamed, and produces scarring (fibrous tissue). This affects its efficiency in conducting electric signals, which then becomes abnormal.
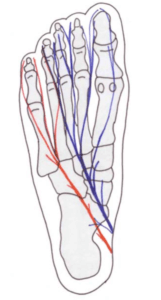
Figen Govsa 2005 anatomy study of connecting nerve branches showed 20% affected the 3-4th toes while 72% had no connection.
Podiatrist turned patient
The toe becomes numb, the small muscles start cramping, the foot becomes painful and the sensations make the brain thinks there is a stone in the shoe. Now we know ladies suffer most, and we know ladies are hosts to footwear fashion, but so is this author. Well, not quite fashion but one shoe that did for me. I had a neuroma because I had the symptoms, localised tenderness was building but orthoses kept me comfortable. This went on for over 4 years, and all was fine until I decided to start cycling seriously. I bought some shoes and started cycling through the winter. Pain, numbness and shooting shocks (paraesthesia) brought me to a realisation the boots designed to lock into the pedals of my bike were the root cause. How can this be? I’m not female by any definition.
I headed off to see my radiologist friend and we undertook an ultrasound and there it was. A steroid injection did nothing and so I was now confronted with seeing another colleague who operated in 2016. It is now 2021.
I have written the book covering my journey and lectured nationally at a Sports conferences and several smaller meetings. Next week (May 12th I am at the NEC and meeting another national meeting of health colleagues). Five more articles later I decided to write this blog for ConsultingFootPain – only this time it is for patients. I wrote an information sheet for those embarking on surgery but like most fact sheets it is only a brief summary. Morton’s neuroma is a painful condition – information sheet. This was a fact sheet I used for patients and it is dated (2018).
The concept of getting the best from fact sheets is important as much as patient articles.

ultrasound is the primary method of checking the presence of a neuroma
What is it?
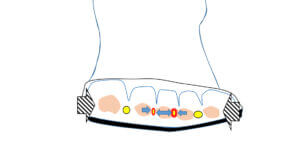
A small nerve (MN) is trapped between the bones called metatarsals and sends electric shock and pain signals into the toes. It can affect one foot or both feet or more than one set of toes.
How do we diagnose this condition?
squeeze test is about 41% sensitive in the presence of a neuroma
What we now know
Nerves can recover but often start off because of local inflammation. The symptoms of what we call neuritis can shoot back up the foot, are often short-lived, and occur when the foot is compressed initially. Most people consult someone between the ages of 40 and 60. However, there are some who experience the condition as early as 20-30. If caught young, then recovery can be encouraging.
In 1995, Gordon Bennett studied 115 patients and followed them for 2 years. Thirty-nine per cent did well with insoles and footwear alterations; in other words, they altered their footwear. Baransel Saygi (2019) found that if steroid was added to using insoles, the benefit increased over 1 year from 11% to 82%. This would only work because the shoes used to accommodate orthoses have to be better than shoes previously used by the patient.
Steroid injections
Steroid injections have been used extensively, and more has been written about the follow-up of large patient groups than any other form of injection. Taken collectively, improvement can be less than 50%. Most follow-ups have not exceeded the 2-year mark. In a 2017 study by Grice (2017), the immediate results shot up to 87% but then dropped to 31% at 2 years.
Clinical evidence
Two excellent papers have been produced, one by Daoud Makki in 2012 and another by Young Park in 2018. Using ultrasound to measure the size of the neuroma, they found that those smaller than 6mm in size respond better than those larger. The normal size of a nerve should be well under 3mm. The size increases because of scar tissue and swelling of the surrounding soft tissues, which remain engorged with inflammation.
Once the nerve has expanded, Sunderland (1953) considered it beyond repair. To make one feel a little more relaxed, some nerves grow, as was found under the more detailed MRI scanning process. Bencardino (2000) identified 33% of her scans had larger nerves, some measuring 10mm. The scientific community has still not answered all of the fundamental questions, but clinicians have tried new methods.
Imaging the nerve
The value that imaging—ultrasound and MRI—brings relates to refining the diagnosis so fewer misdiagnoses are made. The size can be measured, but both methods are not as precise as measuring the damaged nerve under a microscope.
Alternative methods
Radiofrequency treatment under local anaesthetics has gained popularity, and even the government agency NICE has cautiously approved this treatment. Freezing (cryotherapy) appears to have a place, and the results and risks are comparable to surgery. Capsaicin (chilli powder) was used, but the study was too small. Hyaluronic acid (think glucosamine) has been used, but again, there is only one useful study, but this does not mean more research. Alcohol has gained more research recently. This is usually diluted and takes the form of ethanol or phenol. Pabinger (2020) believed that alcohol could shrink the size of the neuroma in some cases. The most extended study I have come across was from Elena Samaila, who used phenol in 125 patients and followed her group for up to 8 years.
Many of the studies conducted have been badly designed and have limited scientific value because patients are not invited into a study as they should be with controls. Many studies look backwards, so controls cannot be applied. For example, many clinicians used steroid injections as well as other methods. Mixing treatment removes the purity of any study.
Di Caprio (2018) reviewed many papers from several researchers and agreed with Gordon Bennett on making sure patients first had conservative treatment. However, it is recognised that unless you can spot symptoms early, many of the suggested treatments fail.
You will notice that pain medicines have not been discussed and are rather more the domain of the GP who, forgive my cynicism, apply pain medicine for feet as a holding mechanism. Sadly, this is old-fashioned; it is unrefined medicine and is part of the problem seen in the UK’s collapsing NHS system because of waiting times. So many conditions require earlier tests (imaging) and treatment to prevent deterioration. Without early intervention, conditions such as neuroma become less manageable and end up with surgery, which, as Di Caprio points out, is, at best, 85% successful.
Stump neuroma
‘A stump neuroma from Morton’s neuroma surgery occurs in the foot, resulting in the surgery removing the Morton’s neuroma. It is a nerve disorder that leads to extreme irritation and swelling in the foot nerves, and it can be excruciating. During the surgery, the nerve is cut, and this can lead to a small growth from the end of the nerve – a ball of nervous tissue, which is known as a Morton’s stump neuroma. It is also called a “recurrent neuroma” as it is a reoccurrence of the initial Morton’s neuroma and it may also be referred to as a “failed Morton’s neuroma surgery”. Morton’s stump neuroma can be a source of great pain for patients. Any type of mild or low pressure exerted on Morton’s stump neuroma can cause pain, which even includes brushing of clothes against the affected site.’ (Pearl, Janet MD, USA)
And so, what happened to my foot? Well, I did well for 18 months, but after surgery, symptoms actually reoccurred. What was around 85% successful dropped to 70% as time progressed. I have been at 55-60% success and have had an alcohol injection, now lasting one month. I have fallen back to my orthoses and get good days.
The ethanol injection was given under local anaesthetic, and for 48 hours, the pain was intense and, at one point, required ibuprofen. I would place my foot at 60% still and my decision for surgery or revision surgery is on hold. Dr Janet Pearl has a suitable site on the subject of Morton’s Neuroma, and I believe it produces some good material. The site was accessed 27/4/22.
What’s the final advice?
In summary, the bottom line is to be wise. If you have pain that affects around or between toes, seek advice. An insole or orthosis is still a valid method. Avoid multiple injections of steroids, as someone is making money if one fails. Two, maybe more – then seek more expertise. This site cannot direct you to anyone specifically, but in the UK, a podiatric surgeon FRCPodS or a specialised orthopaedic foot surgeon FRCS is best. In the USA, go to a DPM podiatrist or a foot orthopedist. The reason for seeing these specialists is because they can provide the full panoply of investigations and have good hospital connections.
If you see a UK GP, ask to see a foot specialist. This is someone who is qualified and trained in medicine, orthopaedics, and podiatry foot health. In the UK, all podiatrists are licensed to practice through a government-recognised register called the Health and Care Professions Council.
You can read my surgical journey in my book Podiatrist Turned Patient: My Own Journey.
Available on Amazon, and you can read the reviews on CFP
Thanks for reading about ‘Morton’s Nerve Pain‘ by David R Tollafield
Modified January 2025
Published by Busypencilcase Communications. Est. 2015 for ConsultingFootPain


Recent Comments