Midfoot Arthritis an often-missed Condition
The Wedding Chat that started it off
Of all places, I sat down at a wedding to speak to an eminent rheumatologist, and we chatted about feet and arthritis. Rheumatology is a medical specialism studying connective tissue disorders. Given that our body is one big connective tissue organ, there isn’t much a modern rheumatologist isn’t interested in. One thing they do is avoid surgery for their patients. Their domain is primarily the musculoskeletal frame. Muscles, joints, and ligaments are their key focus allied to medical organ disease. Speak to any rheumatologist, and they will tell you there are three hundred conditions they might have to diagnose.
As we sipped our beverage to welcome the marriage of my own daughter, I discussed a part of the foot that has lain apart from the daily diagnoses and explained I had set up a clinic to deal with midfoot pain. And so this is the basis of that story. The interest in the midfoot has been recognised by consultingfootpain through one of the most viewed articles – the foot bump, a bony projection causing footwear fit problems.
As a foot specialist, 75% of my workload was dealing with the forefoot, some 15% was the midfoot, and the rest was the hindfoot and the odd knee-foot-related problem.
Discovery of midfoot foot pain
Around middle age, which could be 35 onwards, as a guide, men and women often present with pain across the middle of their feet. There is nothing to see; sometimes, there is no recollection of injury or cause. Swelling is minimal. Mind you, the cowman remembered the animal treading on his foot during milking time, and the industrial worker remembered when his foot was caught on a conveyor belt – as you might gather, the latter case went to judicial review!
In another case, a 35-year-old man feared hospitals and had rheumatoid arthritis affecting his midfoot. This latter case was more interesting as I had to deal with a phobia and offer treatment. It came down to his fear of needles and being awake, so we anaesthetised him, or rather, my anaesthetist did. His pain went, and he felt he had overcome his phobia. This was a great sense of achievement as part of team work.
Imaging
Imaging covers a wide range of investigations. You can x-ray the midfoot and check for bone mineralisation as part of density changes, displacement and fracture. The ordinary X-ray is limited because the midfoot has five keystone bones, mostly square. The gaps are small and overlap. If we take a cross-sectional cut, we must use an MRI or CT scan. This offers inside information.
The Bone Scan or Scintigraphy
I had taken to use a different method in the early millennium. This was known as Technitium scanning and used the same named radioactive isotope. The isotope methylene diphosphonate (MDP) bound with Te99 adsorbs onto the crystalline hydroxyapatite within the bone cells called osteoblasts, representing sites of bone growth. MDP bonds to the hydroxyapatite crystals in proportion to local blood flow and marker an increased bone turnover. A gamma camera records the uptake wherever the bone has active growth.
This is an expensive and time-consuming test but more sensitive than the blood tests I had used previously, such as C-reactive protein. Like many clinicians, writing up research publishing standards takes so long, and recruiting people into a study is a nightmare. The other problem is not just a limited population to select from, but my role in healthcare was to get treatment done!
At an annual conference, I raised my concerns about the midfoot pain mystery, and only one person took note, raising a quizzical eyebrow. It seemed I was alone in my quest to present a picture where I could focus on these small joints and identify a pinpoint specific pain problem. Blood tests are not sensitive, but the isotope was. This allowed me to find the joint concerned. To give the reader some idea of what I was up against, look at the midfoot joints in the illustration below.
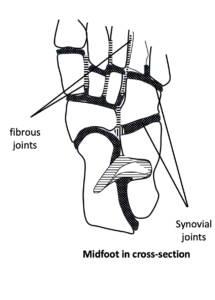
From Tollafield. Fig. 45 An Introduction to the Foot & its common problems in the adult. For foot health practitioners, nurses and health professionals. Amazon. 2023
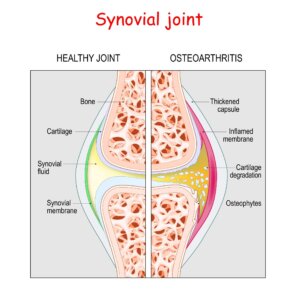
The dark areas are known as synovial joints and, therefore, have a vascular lining – meaning a blood supply. These are typically associated with chronic stress. As the joints share a common association with other bones, several joints can be painful.
Treatment
The joints can be injected under X-ray guidance if there is no fracture or infection. This is carried out under local anaesthetic and only takes around fifteen minutes. Any competent clinician who understanding foot anatomy can perform the tests and offer an injection. Steroid injections are hugely effective and can cure pain. The rider to this is if the inflammation is too great or a different condition co-exists, then the injection may be short-lived.
A second injection will not provide an answer if the first fails. If the injection is in the wrong place, then it will fail. Ideally, the patient does need to be conscious as they can feel the difference between the correct location and one that is not correct. Discomfort is short-lived as the anaesthetic takes over and provides comfort.

The author placed needles into specifically irritated areas of the midfoot using controlled X-ray guidance. Not the jacket protects him from stray radiation.
Alternatives to steroids include sodium hyaluronate as Ostenil, which has promise for some patients. Sodium hyaluronate is found in normal synovial fluid, which bathes joint surfaces and provides some nutrient service.
Attention to basic foot health is important and includes using the right footwear, introducing orthoses to help stabilise these joints and ensuring any repetitive injury is avoided.
Mid-foot pain is manageable, but finding the right person and service to deliver this may be less encouraging. British GPs cannot perform this service without the skill, knowledge and the right diagnostic equipment. Modern ultrasonography opens the window of opportunity, so it is worth conversing with your GP. Those skilled in injecting foot joints include podiatrists, rheumatologists and orthopaedic (foot & ankle) surgeons.
David was a former podiatric surgeon and now an author. You can read more articles on this site or visit Amazon to see his books.
Thanks for reading this article on Midfoot Pain Mysteries by David R Tollafield for ConsiltingFootPain published by Busypencilcase Communications Est. 2015

Published February 2024


Recent Comments