Does Cartilage Damage Impact Treatment?
Cartilage damage in hallux valgus is a common finding. Mapping might offer some predictions regarding long-term outcomes of first toe pathology, or so Thomas Roukis (2005), a U.S. podiatric surgeon, suggests. CFP updates the original article from 2020 with some new material that might allow us to be more objective as podiatric practitioners.
Introduction
It is our view or certainly one held by many, that if we damage our joint cartilage, we are doomed. After 32 years as a (podiatric) foot surgeon, I realised two things. First, most patients recovered even with a bit of stiffness after surgery; secondly, few did less well.
Another factor is that data is skewed toward surgical consultations. Referrals mainly come from medical practitioners who are interested in surgical discussions. Pain, discomfort, and difficulties with walking and wearing shoes are among the 60% of this first-toe condition (PASCOM—Tollafield 2019).
Using RICE, the mnemonic for rest, ice, compression and elevation, might appear ideal, but this is not always practical for patients who do not have acute pain, except for gout or turf toe injury. But what if the pain is associated with a chronic condition? RICE can still be applied, but managing pressure and stabilising the joint form the critical management strategy. Metatarsalgia can be arrested depending on the patient’s footwear considerations with orthoses and insole prescriptions.
What are the objectives of treatment?
There is probably little doubt that surgical papers predominantly refer to cartilage damage in passing without meaningful conclusions. One should ask, does it matter? The podiatrist needs to know how to use the information reliably to inform patients of prognosis. Our information must have a strong evidence base yet be interpreted favourably for the less technical. Based on work by Natalie Joseph-Williams and others, practice guidelines have incorporated new attitudes about patients being able to share their thoughts so they can take part in decision-making. They can only do this if they have information, understand the content and can interpret this to ask questions to which they can contribute. Now, it takes time and preparedness for the clinician to deliver and for the patient to read.
The clinician must use research, interpret the relevant parts, and filter out jargon. This takes time, dedication, and skill. Universities are responsible for showing career degree students how to undertake all these basic skills, and that was one reason why podiatry migrated from a diploma to a degree course.

What intervention is best?
Protecting soft tissue should be paramount, as in footwear, local padding or devices suited to preserving the first to prominence. Splints and taping all play a part, but no one has studied the effect of hallux valgus degeneration from erosions within the conservative arena. It is only once patients present for surgery that the evidence becomes observable. Early splinting is recommended for painful joints, and some outlets sell devices such as day or night splints. Correction of the deformity is impossible, but the painful HV joint can be helped considerably. Plaas researched and found positive benefits from a commercially available design that is more expensive than simple forms. The illustrated example allows adjustment and walking. When considering the lack of information on conservative care, the best insight into the effect of treatment comes from Grice et al. (2017). This paper helps identify the concept of timeline by recording the limitations of steroid injections.
The problem with Grice’s steroid injection study is that it is specific for hallux rigidus (HR) rather than hallux valgus. In his study of 365 injections for ankles, plantar fascia, neuroma and synovitis, HR drops from 92% to 9% over one year, meaning the benefit is poor. However, synovitis in lesser mtpj’s delivered 80% effectiveness initially and remained at 31% at the end of the year, a 90% reduction compared to a 61% reduction. Soft tissue does not do better. Plantar fasciitis dropped by 93% versus 64% for a neuroma.
Evidence from Imaging
Bock et al. (2004) looked at the reliability of X-rays against two methods of recognised evaluation. The Kellgren-Lawrence scale 1-4 shows different levels of deterioration by radiographic interpretation, and secondly, the International Cartilage Repair Society scale (ICRS; 1998). In an ideal world, there should be a reasonable comparison, but 54% (144) underestimated the presence of degeneration, and 11% (29) overestimated the presence of degenerative changes. Around 35% (92) agreed with the intra-operative scale using the ICRS. Table 2 shows the Kellgren-Lawrence scale for radiographic interpretation of damage in hallux valgus.
Magnetic Resonance Imaging (MRI) is still in its early stages of use for hallux valgus. This is clearly due to cost and access even in strong health economies. The MRI, however, is the ‘go-to tool’ in orthopaedics (Choi et al., 2018). Of the MRI, they state, ‘The most common findings observed in hallux valgus were hypertrophic medial eminence (95%), sesamoid proliferation (90%), and adventitial bursitis (90%). They also found that osteophytes (77%), subchondral cysts, and bone marrow edema were commonly found with hallux rigidus.’
Intra-articular investigation or arthroscopy is probably still in its infancy compared to knees and ankles. Fibre-optic cameras are now small enough to insert into the mtpj, as recorded by Lui (2008) cited by Villas (2012). Synovectomy produced a 90% good outcome in a study with 121 patients.
Mapping Cartilage Lesions

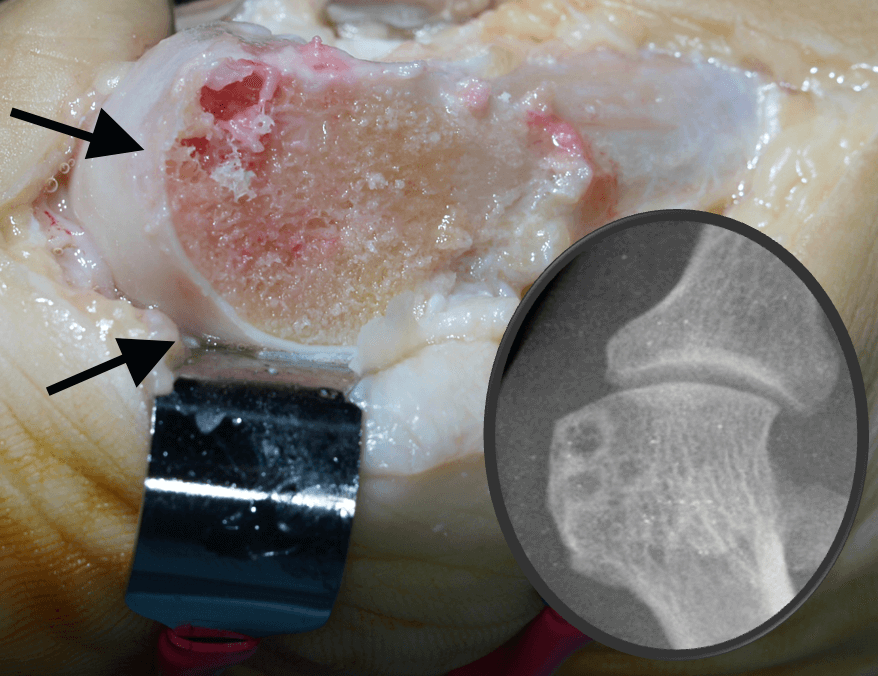
International Cartilage Repair Society score 1-4 as in first toe joint.
Roukis et al. (2005) provided the first mapping exercise on live patients rather than cadaveric studies. Such studies may have predominated previous work on cartilage defects (Scranton & Rutowski,1980), where sesamoids were blamed for erosive changes. The top layer of cartilage, the pearly white material (lamina splendens), measures in microns, while the cartilage thickness for the first toe joint is less than 1mm. The chondrocyte content is low (0.4-2%), relying on the specialised effect of collagen fibres, proteoglycans and water. The two deeper zones do not directly affect dealing with stress.
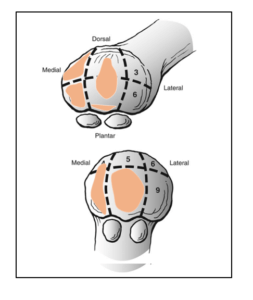
Common areas of erosions across all papers. Adapted by the author from Jastifer et al. (2014)
Any replacement repairs with fibro-cartilage, Walsh et al. (2007) rather than new cartilage. Adaption to cartilage and bone is seen around the dorsal and medial aspects of the metatarsal head within the first mtpj anatomy. Roukis et al. (2005) suggested that erosive cases existed in 100% over 50 in a study of 120 patients affecting one or other part of the mtpj. Jastifer et al. (2014) found that 91% of his patient cohort had osteochondral lesions in 56 consecutive feet. The numbers may appear low compared to a study by Bock et al. (2004), who reported 73% of their 196 patients with erosions. Jastifer used the ICRS scale, while Roukis did not. Jastifer followed his patients for 2 years and measured the damage across the cartilage surfaces for sesamoids and metatarsals.
Are we any better informed?
Bock (2004) compared radiology and cartilage damage against the backdrop of X-rays. Only 35% of X-ray interpretations agreed with the intra-operative findings along the lines of ICRS; 54% were overestimated, and 11% were underestimated. This means X-rays are unreliable for evaluating arthrosis in hallux valgus, more so for HR.
Roukis considered a 13-zone map, while Jastifer only used nine zones, but both concluded standard zones were affected. Roukis used measurable parameters such as angles between common joints and bone relationships, hoping to indicate which presentation might afford a greater predisposition to erosion, but felt that such angles did not predict the incidence of likely lesions. Jastifer (2014) does not wholly agree with Roukis on the deformity angles and their relationship with erosions.
Although 6 years old, Jastifer’s paper (2014) is the latest in a small series on the first MTP joint erosions. Their conclusion, however, suggests that the cartilage lesion’s grade and the lesions’ extent do not strongly correlate with the deformity’s severity. And yet, we know that the number of lesions found increases as the deformity increases. Jastifer found similar findings for the most frequent locations. The medial inferior and superior zones held the most significant frequency, but this was not universally found among all authors.
Medial wear was considered due to compression forces, rotation of the metatarsal head as the deformity increases and the effects of medial ligament strain. As the deformity leads to subluxation, could the loss of the integral lubrication system lead to desiccation and easier tangential wear? Disuse atrophy is widely recognised alongside the medial sagittal groove.
Subchondral bone cysts (see the main article picture) arise when the surface thins and the synovial fluid is forced into the Haversian canal with bone. When removed, the cysts form jelly-like substances and exhibit a lining within the cavity. The cysts do not affect patient treatment outcomes, although large cysts could lead to fractures. X-rays show an area of dark change or lucency where cysts are apparent.
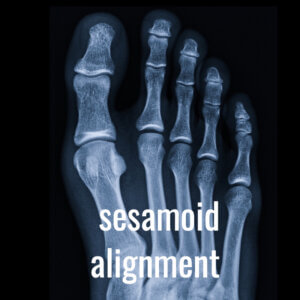
Grading 1-7 relates to the position of the tibial sesamoid. Positions 2-3 are shown.
The illustration of an X-ray taken standing shows that at positions 2-3, the tibial sesamoid is close to abutting the crista even though there is a good joint space. The alignment appears sound, but the X-ray does not account for any frontal plane rotation.
Metatarso-sesamoid articulation
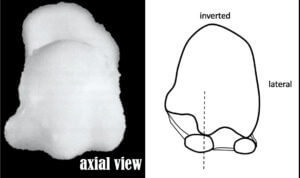
relationship of sesamoids and metatarsal
Sesamoid displacement is easy to assess from X-rays, but the correlation with actual erosive changes is less straightforward. Males showed more erosive zones when a demarcating map drew 13 different locations, Roukis. As the age of the participants increased, the number of zones involved increased, and the incidence of a lesion increased. Fewer erosions were seen when the first toe was shorter than the second digit, Roukis et al. (2005). Medial erosions predominated, while the lateral side was spared more often.
The proximal articular set angle, or PASA, was associated with the inferior central zone erosions. This is an angle of the head of the cartilage cap upon the first metatarsal. It has been considered adapted in shape and position over time and as part of development. Breslauer et al., 2001, used cadaveric studies and applied them to patients to show that the metatarsal rotated to increase sesamoid impingement against the crista.
Getting closer to the answer?
Jastifer makes an important statement; ‘Patients should be counselled about the prevalence of these lesions when discussing expectations from surgery but no less the role of the sesamoid articulations.’
The Tibial Sesamoid Joint plays a part in sesamoid pain and surgical outcomes. Jastifer followed patients for 24 months, and those with 21 degrees of hallux valgus returned a good result in 83% of cases. Those under 21 degrees were 100% satisfied. This seems surprising when Jastifer found in 51 of 56 feet a mean score for 50mm2 surface area damage using callipers. Grades 2 and 3 for depth prevailed across most studies. Yet, the general view is that the surface area and depth of lesions do not contribute to the outcome after treatment. Level 4 means the bone and vascular tissue are involved and create haemarthrosis, where fibrin infiltrates the synovial fluid and fibrils form a web across the joint. This limits movement and can tear at the remaining cartilage tangential or superficial cartilage zone.
If the synovium becomes inflamed, it cannot remove inflammatory debris, and if blocked by a fibro-cartilage or bony osteophyte, synovial lubrication fails. A breakdown in the mechanism associated with the extracellular fluid transport mechanism and surface lubrication that limits friction sets up the process for further damage.
The Critical Features Seen in Hallux Valgus
- Degeneration of cartilage needs to be at a late stage 4 with haemarthrosis
- Osteophyte change in bone impedes synovial lubrication
- Bone marrow damage does not play a substantial part in the success of the treatment and appears as part of pathological features rather than symptoms
- Subchondral bone sclerosis may add to the pain but also form pathological changes
- Synovial proliferation upsets lubrication and the welfare of cartilage
At least two of the above must combine to affect a joint’s declining health and cause irreversible changes in mechanical and chemical terms.
The latest book on bunions is available and more comprehensive than ever, answering those questions that most GPs are unable to offer. Amazon as an ebook costs £5.20 and paperback costs £12.99. Colour hardbound copy £32.00
Thanks for reading ‘Cartilage Damage in Hallux Valgus’ by David R Tollafield
David is a full-time author and has retired from podiatry practice
Published by Busypencilcase Communications Est. 2015 for ConsultingFootPain
Modified January 2025.

Trackbacks/Pingbacks