Swellings in Feet Can be Confused with Ganglions
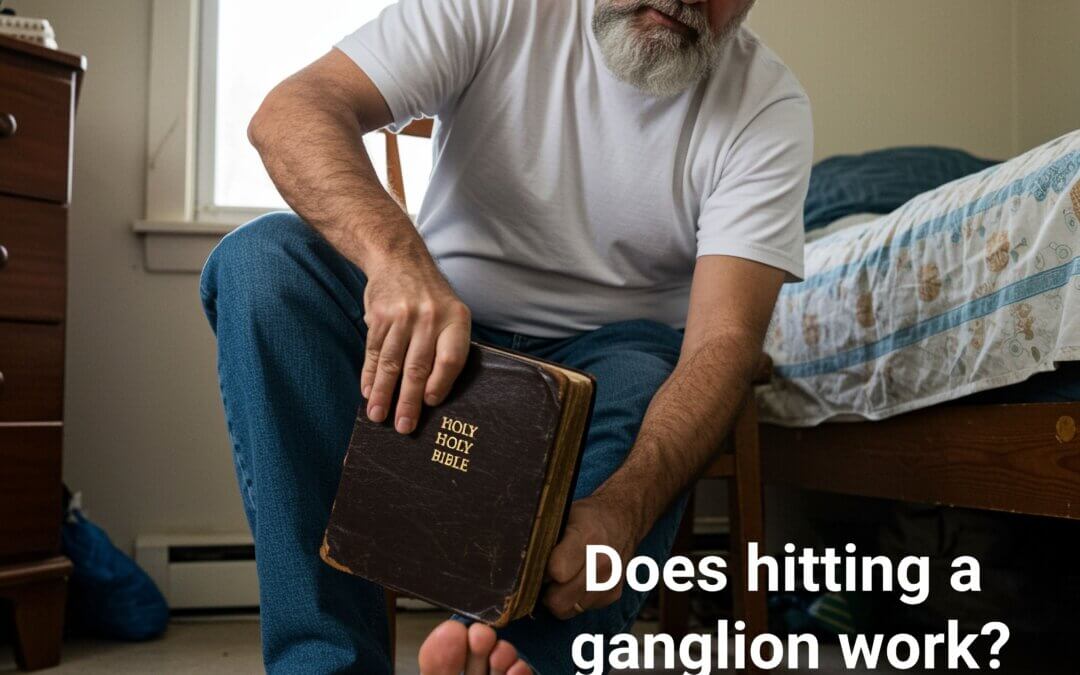
You see a soft swelling on the foot, and someone tells you it’s a ganglion. Should you hit this with a book, like the Bible? This was often the most accessible book, and everyone had one in the house, so it had nothing to do with religion. Of course, the answer is no. Hitting any tissue is not recommended, and indeed, one should avoid using computer tablets and iPads in place of the Bible – that is, unless you are searching for information such as this site, then hit the keyboard instead.
Keywords: Ganglion, bursa and mucoid cyst
Small swellings often do not bother us, but those that are unsightly and cause shoe-fitting problems start to niggle. Until I became a foot surgeon, I was probably as ignorant as any, except I knew what the textbooks said. The mantra from the orthopaedic lecturer was enshrined in surgical removal under general anaesthetic and a tourniquet. Having managed many by injection, aspiration (draining fluid off), and surgically removing all manner of cysts has led me to a clearer thought process.
If it doesn’t hurt, doesn’t get bigger or interfere with life, leave it alone.
Cysts
Mucoid cyst
The word cysts implies swelling, and cysts have the unique feature of having fluid inside. In the foot, we see a cyst walled off under the skin with a lining called a capsule. Take the so-called mucoid cyst because of its mucinous fluid content; the small digital joints (interphalangeal spaces) are damaged and leak, forming the characteristic swelling that can be taken as an arthritic (Heberden’s node). It does not mean someone has arthritis, but it remains a common finding in feet and hands.

MUCOID CYST TYPICALLY AFFECTS DIGITAL JOINTS IN FEET
Pilonidal Cyst
A ganglion and a bursa are both examples of cysts, but what about the foreign body that forms a swelling? One that arises occasionally is the inclusion cyst, where a foreign body penetrates the skin and closes over, such as the pilonidal cyst. A simple animal hair or a small piece of glass will set this off. The giveaway is that the pilonidal cyst usually arises on the sole. If we incise the cyst under anaesthetic, sterile pus is often apparent. This material is the byproduct of something the body recognises as alien and battles with its white blood cells (leucocytes). The end result of the battlefield is this white material that has a caseous (cream cheese) content.
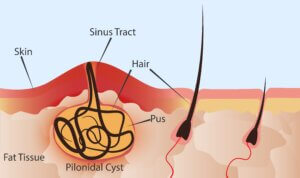
PILONIDAL CYST
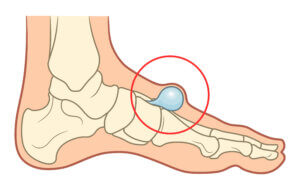
Bursal Cyst
The bursa is another cyst that can form in the foot to protect tendons, such as the significant achilles tendon against the heel bone. The deep anatomical bursa can become inflamed but settle. An adventitious bursa is another cyst that forms from tissue damage caused by pressure and is commonly seen on the sole. If this is opened up, unpleasant blood-stained material can ooze out and, when examined under a microscope, show inflammatory cells being active.
Ganglionic Cyst
Then we have our ganglion, which again forms like the anatomical bursa, but unlike this bursa, it appears more like a mucoid cyst. The thin gossamer lining has a thin or thick, clear, fluid-like gel. The lining contains another part of the anatomy that can secrete a synovial-like fluid. While many might assume this could be related to gout, this is not the case. Gout forms more of a localised hard swelling with a greater coloured skin flare, while the inside has a thick white material like crushed almonds.
Some of the tendons have a secretory lining and can tear. These tears are so small that you cannot see them on ultrasound scans unless the fluid and lining are large, forming the catch-all term – cyst. Just because you may have cysts elsewhere in the body does not imply any relationship with the ganglionic cyst, sometimes known as a synovial cyst.
The skill is determining what the swelling is
Where Do We See Ganglia in Feet?
In front or on the side of ankles, around the back of the heel, on the top of feet, on the side of feet. Over, the big toe, a ganglionic cyst, becomes part of the all-encompassing bunion. While harmless, in many cases, all swellings should be checked and treated by a specialist rather than a GP. Of course, this depends on access to a professional. Ganglia can descend deeper toward the joints, and simply sucking off the fluid alone is pointless in the long term. While local anaesthetic will often be deployed sometimes, because of difficulties in anaesthetising the deeper tissue, a general anaesthetic is required.

Hitting a ganglion with a heavy book will reduce the swelling as the thin lining collapses. A heavy book might have worked if the additional trauma did not lead to fractures! Reformation of any membrane can return if the derivative tissue remains because this has not been removed. Many ganglia do resolve and absorb, so surgery is not essential in all cases.
Ganglia and bursae often appear together in conversation. They are different, although they present similarly as visual swellings under the skin. Bursae are usually found around pressure points or where pressure builds up. The deeper tissues are damaged by friction and shearing forces that tear. Again, joint linings and tendons can be involved, but the content differs. Ganglia have thin linings, while bursa balloon-like pockets are flat and have thick linings. You do not have to have arthritis to have a bursa.
Unlike a ganglion, a bursa is not easy to spot from the outside. Those with experience will usually seek an ultrasound image, as these are not picked up with an X-ray. A ganglion is often balloon-like and spongy to feel.
The nuisance factor is more common than pain unless nerves are trapped, signified by sharp electric shock pains that shoot into the foot or up the leg. Tapping the nerve can elicit this sign, called Tinel’s sign. Infections are not common, but where pain is noted or increases, the swelling must be investigated and managed. Deeper bursae do well from injections, where they form part of normal anatomy, while chronic bursae do not on account of becoming established.
Any swelling in the foot that enlarges should be evaluated by a second opinion. This opinion should be sought from medical doctors or medically trained people, such as specialist podiatrists.
-
-
-
-
-
-
-
- Take a photo, measure the size and monitor any change over a few weeks.
- Wear different shoes to avoid taking pressure.
- If painful, seek an opinion earlier.
- Do not try to burst, pop, or prick a swelling.
- Malignancy is rare, but can arise.
-
-
-
-
-
-
Thanks for reading ‘Why Can’t You Make Ganglions Disappear?’ by David R Tollafield
David is a full-time author and former podiatric surgeon and writes for Busypencilcase Communications under ConsultingFootPain. In his former career, he specialised in foot pathology, histology and chronic pain management.
His publications are written to guide patients and professionals. You can view his books at davidtollafieldauthor.com or follow him on Facebook @davidtollafield and X @myfootjourneys
His latest guidebook was launched in January 2025
available from Amazon as an ebook, paperback or hardback
Published by Busypencilcase Communications. Est.2015 for ConsultingFootPain
February 2025

Recent Comments