Is it true you can make a ganglion disappear?
Ganglionic, bursal and mucoid cysts are discussed in this short article. You see a soft swelling on the foot, and someone tells you it’s a ganglion. Immediately, you might be persuaded to hit this with a book. The Bible often represented an accessible book and had nothing to do with religion. As the anecdotes came from a time when the UK was predominantly Christian, other representative religious groups were not mentioned as in the Koran (Qu’ran – Moslem), Torah (Judaism), Tipitaka (Buddhism) or books (poems) used by Hindus. In modern parlance, there are plenty of sources of heavy books. Still, any form of hitting tissue is not recommended, and indeed, one should avoid using computer tablets and iPads in place of the Bible – that is, unless you are searching for information such as this site.
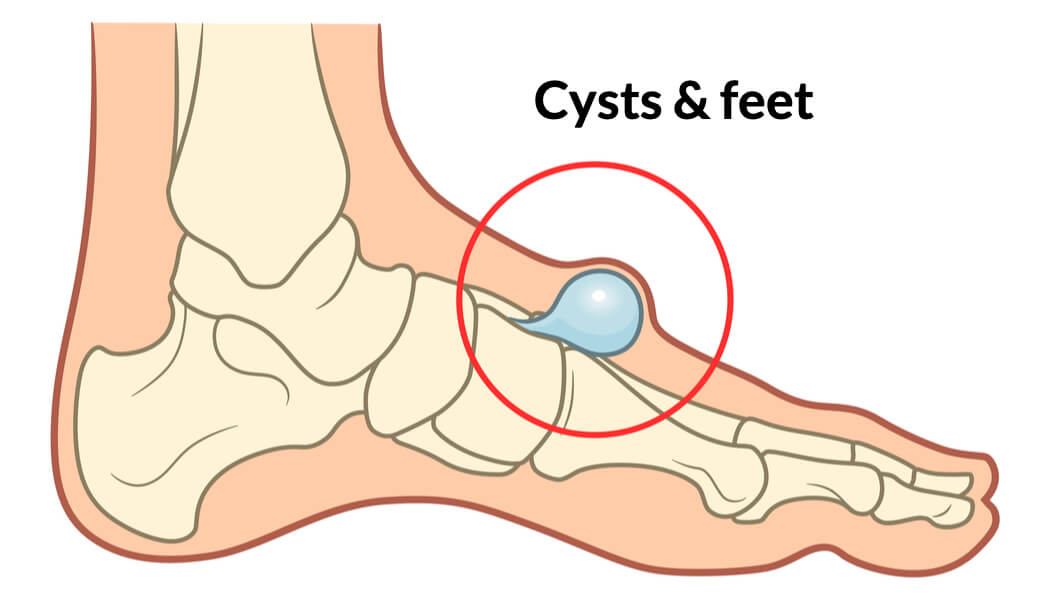
We have seen ganglions related to a bunion, but they can arise over the top of the foot, the side of the ankle, and even the back. The thin gossamer lining has a thick, clear, fluid-like gel. The lining is usually part of another part of the anatomy that can secrete a fluid, often synovial in nature. This is because the joint lining known as the capsule can tear and leak. Some of the tendons have a secretory lining and can tear. These tears are so small that you cannot detect them on ultrasound unless the fluid and its lining are large, forming the catch-all term – cyst. Just because you may have cysts elsewhere in the body does not imply any relationship with the ganglionic cyst, sometimes known as a synovial cyst.
Where do we see ganglions (ganglia) in feet?
In front or on the side of ankles, around the back of the heel, on the top of feet, on the side of feet and even the toes can produce these swellings. In the toes, the cyst is usually known as a mucoid cyst. While harmless, in many cases, all swellings should be checked and treated by a specialist rather than a GP. Of course, this depends on access to a professional. Ganglia can descend deeper toward the joints and simply sucking off the fluid alone is pointless in the long term.
Hitting a ganglion with a heavy book will reduce the swelling as the thin lining will collapse. A heavy book might have worked if the additional trauma did not lead to fractures! Reformation of any membrane can return if the derivative tissue remains because this has not been removed.
Ganglia and bursae often appear together in conversation. They are different, although they present similarly as visual swellings under the skin. Bursae are often found around pressure points or where pressure builds up. The deeper tissues are damaged by friction and shearing forces that tear. Again, joint linings and tendons can be involved, but the content differs. Ganglia have thin linings, while bursa balloon-like pockets are flat and have thick linings. The inside of a bursa can have various types of cells instead of jelly-like clear fluid. The discharge may be white, afforded by blood cells trying to mop up the damage. Bursae appear under the foot, around joints, especially in the front of the foot. They can arise in association with inflammatory arthritis, which is a medical condition. You do not have to have arthritis to have a bursa.
From the outside a bursa is not easy to spot and those with experience will usually seek an ultrasound image as these are not picked up with an x-ray. A ganglion is often balloon-like and spongy to feel.
Damage from cysts
Bursal cyst: as time progresses, a bursal cyst deteriorates and damages surrounding tissues under constant pressure. A 75-year-old had a sizable bursa left to develop over 20 years. She had originally had surgery on her big toe, and this was fixed in an unfortunate position many years earlier. The toe stuck up, and the pressure under her joint was immense, destroying the padding, fat, and surrounding connective tissue, which formed a cyst. There was minimal padding upon surgical removal, although she was given a spongy insole. This case was extreme, but many patients presented to my clinic with cysts of this nature and required surgery. Those diagnosed with severe rheumatoid arthritis formed unpleasant cysts filled with inflammatory soups that could be yellow or white. This destructive disease would leave joints dislocated and disrupted, affecting anything in the way, like a forest fire attacking all vegetation.
Mucoid cysts over the small toe joints in the foot can be left unless troublesome and seldom cause extensive damage as they only trouble people with shoes that rub. Blob-like appearances may have discoloured appearances, but the fluid varies in thickness and is harmless. Steroid injections and sucking off (aspirating) fluid can help, but returning cysts can enlarge over the interphalangeal joints. Larger cysts, if removed, require a small part of the joint taken away, which has no long-term problems but may shorten the toe slightly. The fingers on the hands are also affected but do not suffer the problems imposed by footwear rubbing. If the toe is hammered (bent), then, of course, this would ideally be best fixed.
Ganglionic cysts tend to become a nuisance in tight shoes that press against bone. They occur commonly with big toe deformity (hallux valgus). The ganglion is a bunion and often has an enlarged piece of bone lying underneath called an exostosis. Ankles are the most difficult to manage as the lining is often very deep. Special scans called MRIs can help determine the extent of involvement. Surgery is more complex and should not be seen as simple as nerves can become entrapped. Additional blood vessels will add a further complication and have to be sacrificed where long-term damage has caused extensive scarring. Even surgical removal around the hindfoot can miss all the fragments and membranes left can reignite more cystic sacs. The adage taught to undertake ganglion removal under general anaesthetic, and tourniquets are untrue, but modern regional anaesthetic techniques can be used instead of the knock-out technique. The surgeon faces a very thin lining, which nearly always ruptures, and tracing all ganglion elements requires careful exploration for missing elements.
Do bones cause cysts?
Indeed, this is the case, but these are either picked up when the foot is x-rayed for another problem or unexplained pain arises. Bone cysts are similar in that they have a lining and can produce mucoid or fatty content. The bunion-hallux valgus deformity frequently has an underlying cyst called a Goede’s body radiographer. The reason for this is the stretching of the inside ligament as the big toe leans more and more toward the small toe. Large cysts can be filled with patient bone, but their lining must be cleaned out. Cysts affect all bones, but the heel bone (calcaneus) is a frequent target, albeit rare.
Pain and symptoms
The nuisance factor is more common than pain unless nerves are trapped, signified by sharp electric shock pains that shoot into the foot or up the leg. Tapping the nerve can elicit this sign and is called Tinel’s sign. Infections are not common but cause ascending pain and must be investigated and managed. Deeper bursae do well from injections where they form part of normal anatomy. These are called an anatomical bursa. Tethering down with strapping can help or they can be protected by foam and gel padding.
Naturally, no one wants surgery. Any swelling in the foot that enlarges should be viewed with a second opinion. Online opinions may be a good idea from those willing to offer such a service, which may be free or charged at a low cost, saving money. An opinion should be sought from medical or medically trained people, such as podiatrists.
- The two biggest tips are taking a photo, measuring the size and monitoring the size over a few weeks.
- Wear different shoes to avoid taking pressure.
- If painful, seek an opinion sooner.
- Do not try to burst, pop, or prick a swelling.
- Malignancy is rare, but it does arise.
Thanks for reading ‘Understanding Ganglions in Feet’ by David R Tollafield
Adapted from Foot Health Myths, Facts and Fables by the same author and now available on Amazon as an ebook and paperback
David is a full-time author and retired podiatric surgeon
Published by Busypencilcase Communications. Est.2015 for ConsultingFootPain


Trackbacks/Pingbacks