Cryosurgery and Radio-frequency ablation
Morton’s neuroma series
Thermal or surgical choices for Morton’s Neuroma are in short supply of long term evidence. So we must ask ourselves. Is surgery successful, and should I know more about what to expect? In addition which surgery is best – if there is such a thing? And, is there an alternative to surgery? It is in this area we need to explore the other possibilities.
Having covered cause, diagnosis and conservative care in previous articles, there is a middle stage. Injections, guided with imaging or without imaging, will have been offered by most clinicians before breaking the skin. Surgical intervention has always been the last resort but there is a growing inclination to use newer modalities that require local anaesthetic with thermal destruction or ablation. These are chiefly cryosurgery, radiofrequency and laser. Extracorporeal treatment has little evidence as does laser so we must await more research of a quality that offers assurance (Thompson 2020).
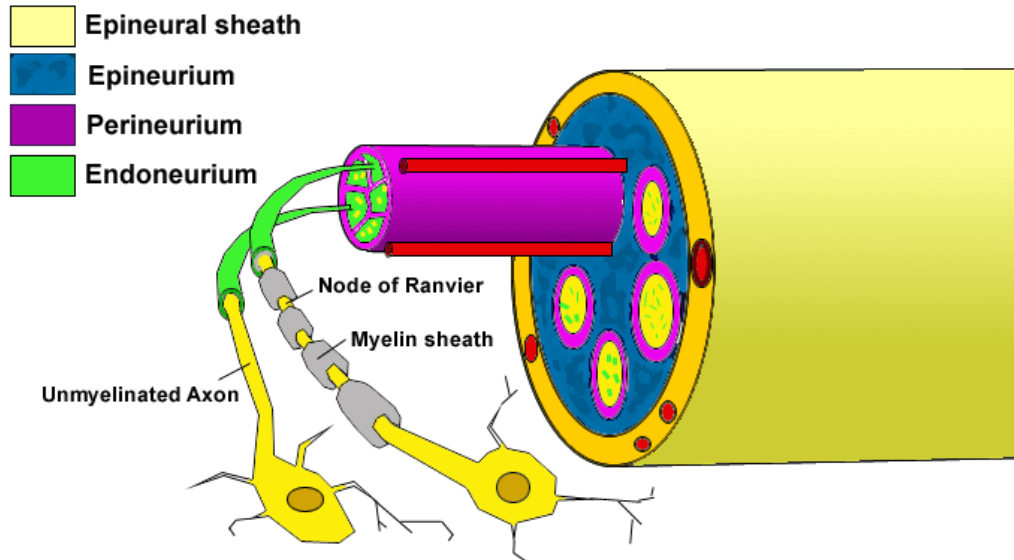
Cryoablation and radiofrequency are but in name surgical procedures as they require considerable care with sterility, imaging support at the time of treatment and anaesthetic of one form or another. The risk element is heightened by thermal (heat or cold) damage to adjacent tissues. The evidence, while encouraging is limited at this time, often represented by smaller study numbers.
In some cases, other interventions have confounded the results. Mixed injections with steroids for example can skew data a little when looking at pure interventions from a scientific standpoint. DiCaprio (2018) points to conservative care being perhaps 30% successful but we know that in many cases this is because treatment commences late and diagnosis has been predicated on the patient coming forward in a timely manner to allow better exposure to mechanical means.

Cazzato 2018 Cryoablation under MRI showing T1 weighted scan and dark area ice ball from technique under local anaesthetic
Cryoablation or cryoneurolysis (CA)
Cazzato (2016) used a small study of 20 patients and performed cryoablation under local anaesthetic with MRI guidance. The latter imaging is fairly novel for a pedal complaint. Visual analogue scales (VAS) were employed and a 4-point satisfaction questionnaire (Johnson). Patients with previous failed conservative management were offered CA.
A single therapeutic freezing cycle lasted 150 secs creating an ice ball which was monitored using multiple coronal and sagittal T1-weighted sequences throughout the procedure. The procedure time was around 40 minutes with complete satisfaction of around 77%. A single complication of superficial cellulitis was reported at the probe entry through the skin. The authors concluded this was a novel therapy requiring further prospective studies.
Friedman (2012) perhaps was one of the initiators of this technique for sural lesions. Cazzato believes that CA could avert stump neuroma. At the time of writing NICE (UK) does not publish any recommendations or reviews on cryoablation and it seems that this treatment is still considered on a trial basis despite this being offered in the UK and yet there are podiatric clinics set up now offering dedicated care with this method.
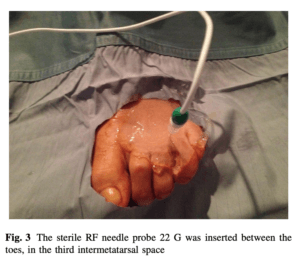
After Masala 2018 radiofrequency probe is essentially a percutaneous surgical technique.
Radio-frequency (RFA)
The most recent paper covering radio-frequency ablation (RFA) was reported in 2018, Salvatore Masala from Italy with earlier papers; Paolo (2008), Chuter (2013) and Deniz (2015). Paolo showed an 89.6% VAS score reduced for 32 neuromata, Chuter 87% satisfied for 30 neuromata and Deniz 60% satisfied for 22 neuromata.
Thomson (2020) believed the follow up of 9 months was short and again confounding factors attributed to using corticosteroids, reduced the value of the studies. Where the procedure was performed in operating theatres these had been excluded. Such exclusions prevented Masala’s review from being included in the systematic review although this was recorded as a prospective level review. As with many reports, Masala’s paper came from an interventional radiology unit rather than orthopaedic source. Sterile preparation was performed on patients aged between 33-75 and predominantly female: male (46:6). VAS and foot health status scores questionnaires (FHSQ) were used and followed up at 7 days, 2,6 and 12 months. The recorded size of the lesion indicated 69% >5mm.
Masala looked at body mass index (BMI), walking activity, footwear and foot type. The latter was divided into normal, pes valgus and pes cavus. The clinical characteristics when analysed for the study numbers showed no statistical significance as the results overall showed no distinct differences when RFA was performed. No complications were reported in this study but we know that other studies have shown complications around localised post-treatment pain. VAS scores dropped and were maintained over the course of 12 months and the Foot Health Satisfaction questionnaire (FHSQ) scores increased. NICE guidelines approve RFA but expect local NHS trusts to be informed for governance purposes. The report on evidence does not cite the papers or evidence level.
“Radiofrequency ablation (RFA) for symptomatic interdigital (Morton’s) neuroma is a percutaneous treatment, which is usually done as an outpatient procedure under local anaesthesia. Using imaging guidance, an RFA probe attached to a generator is inserted into the web space between the toes and into the area of the neuroma. Controlled pulses of radiofrequency energy are delivered, which causes thermal ablation of the nerve. After the procedure, a steroid injection is usually given to reduce pain and inflammation. Patients are discharged as soon as comfortable and advised to limit their walking for 1 or 2 days. Any pain is managed with analgesics. The procedure can be repeated if necessary after a few weeks.” (NICE accessed 31/10/21. Last Published 16/12/15) See appendix for an evidential summary from NICE.
In a second paper by Connors (2020), a podiatrist looked at a retrospective follow up with an average of 2.6 years conducted on 32 patients. Ten patients had had corticosteroid treatment before entering the study. The original study had 58 cases but some loss occurred from the initial cohort identified for RFA. AOFAS and pain scale assessment scores were recorded. More than 1 treatment was necessary with 11 (35%) not improving after a single treatment of RFA. Only 3% (9) had three treatments without success. The number of exposures was 2-6 otherwise where 17 (53%) recorded excellent results. Like many papers, there are inconsistencies in exactly how success was measured and what cut off points were used which highlights the problems with retrospective analysis.
Appendix 1 – NICE evidence
1) A case series of 25 patients (30 feet) with symptomatic interdigital (Morton’s) neuroma reported a statistically significant reduction in pain scores on activity after ultrasound‑guided radiofrequency ablation (RFA) treatment. Pain scores were measured on a visual analogue scale (assessed on a scale of 0–10, with lower scores indicating less pain) and were an average of 6.0 at baseline compared with 1.7 at 6‑month follow‑up (p<0.001).
A case series of 37 patients (38 neuromas) for whom conservative management failed and who had RFA, reported median numerical pain scores (assessed on a scale of 0–10, with lower scores indicating less pain). Pain scores decreased significantly from 9.0 at baseline to 5.0 at an average follow‑up of 10.6 months (p-value not reported).
2) The case series of 25 patients reported that the average overall symptom improvement (as described by patients, not otherwise defined) was 76%. The case series of 37 patients (38 neuromas) reported that for 74% of neuromas there was a complete or partial resolution of symptoms and for 26% there was no benefit at an average follow‑up of 10.6 months. All patients with neuromas in the third web space (n=18) reported complete or partial relief of symptoms compared with only 50% of those with second web space neuromas (n=20).
3) The case series of 37 patients reported that 87% (32/37) of patients were satisfied with RFA treatment at an average follow‑up of 10.6 months. Most patients (84%) said that they would have the procedure again.
4) The case series of 37 patients reported that 2 patients with no symptom relief had repeat RFA treatment but were not satisfied with the outcome at an average follow‑up of 10.6 months.
5) A case series of 29 patients (with 32 neuromas treated) reported symptom recurrence in 1 patient at a 9‑month follow‑up. This was successfully treated with an injection of steroids and local anaesthetic.
6) Progression to surgical removal of the neuromas was reported for 29% (11/38) of neuromas
7) Neuromas in patients with partial symptom relief and 8 neuromas in patients with no symptom relief) in the case series of 37 patients (38 neuromas) at an average follow‑up of 10.6 months. Of the patients who had surgical removal, 6 patients had complete relief of symptoms, 3 had partial relief, 1 had no change in symptoms and 1 got worse. The average numerical pain score decreased from 6.9 to 2.7 (p-value not reported).
For references for this series please select the LINK
NICE https://www.nice.org.uk/guidance/ipg539/chapter/3-The-procedure
- Cazzato, R.L., Garnon, J., Ramamurthy, N. et al. Percutaneous MR-Guided Cryoablation of Morton’s Neuroma: Rationale and Technical Details After the First 20 Patients. Cardiovasc Intervent Radiol 39, 1491–1498 (2016). https://doi-org.libaccess.hud.ac.uk/10.1007/s00270-016-1365-7
- Masala, S., Cuzzolino, A., Morini, M. et al. Ultrasound-Guided Percutaneous Radiofrequency for the Treatment of Morton’s Neuroma. Cardiovasc Intervent Radiol 41, 137–144 (2018). https://doi-org.libaccess.hud.ac.uk/10.1007/s00270-017-1786-y
- Connors, JC, Book, AM, Rao, N, Kingsley, JD. Radiofrequency ablation for the treatment of painful neuroma. J.Foot & Ankle Surg. 2020;59:457-461
Thanks for reading ‘Thermal or surgical choices for Morton’s Neuroma?’ by David R Tollafield
Available from Amazon books as an ebook or paperback
Why not read the sixth article Incisional Surgery for Morton’s Neuroma
Sign-up for here my regular FREE newsfeed
Published by Busypencilcase Communications. Est. 2015 for ConsultingFootPain



Recent Comments