The Deforming Hammer toe – Part 1
Self-help for toe problems
My journalistic head spun when a neighbour (Zandra) appeared on my doorstep asking what to do about her second toe. We needed a bit of research, and looking at the problem from my 43 years as a podiatrist, I knew more information could help readers. Having had a successful bunion surgery some time ago, Zandra found her second toe bent. What could she do? Why did this happen after surgery?
CFP always tries to enlighten readers and provide self-help advice where possible. In other cases, a reader must be directed to a professional, but ideally with some background knowledge first.
 Background to Case History
Background to Case History
Zandra’s second toe, the index toe, bent sometime after she had her first toe (bunion) surgery. Originally she had surgery in 1969, then a revision in 1976. Patients are warned that bunion surgery before age 30 can lead to early reoccurrence (Tollafield, 2019). By 2015 Zandra was back to consult her foot surgeon. It was now the recognition she had toe problems. She shared her consultant’s letter dates 9/4/2015. The notes stated: RECURRENT LEFT HALLUX VALGUS & TRANSFER LOADING LEFT FOREFOOT LEADING TO MTPJ2 SYNOVITIS/ARTHRITIS. A guided injection was used to treat both the joint and a neuroma. Orthoses were recommended. In Part 2, I will provide academic evidence for hammer toes but in Part 1, let me start with the chief problem and then deal with the solution for Zandra.
From my examination in 2022, Zandra had a predominantly hammered second toe with residual drift of the first toe. However, the lesser third toe was also bending (flexion). In podiatric-orthopaedics, we talk about hammer, claw and retracted toes. CFP published a general article called Hammer Toe Sounds like it belongs in a Tool Box in July 2020, covering toe deformities in a broader sense. There are three joints attached to the foot – at the nail end, the distal interphalangeal joint (DIPJ), the middle posterior interphalangeal joint (PIPJ) and then attaching the toe to the metatarsal, the metatarsophalangeal joint (MTPJ). Thirty-nine years after her second surgery, she developed transfer problems. The pressure (load) under the forefoot (ball) had developed symptoms (metatarsalgia). The toes appeared to adapt with their tendon (guides) as time progressed.
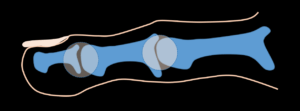
Examination today (11/22) illustrates the problems. Interestingly, the right foot also had surgery in 1969 but has not developed the same concerns. The left second toe is shown hammered at the PIPJ but lifted at the MTPJ. The third toe is hammered at the PIPJ but not lifted at the MTPJ. The fourth toe, called a mallet toe, is flexed at the DIPJ alone.

With permission (author), Zandra’s left foot
The pressure created by flexed toes is the presence of a corn within the callus at the apex. The picture is slightly out of focus, but the second toe does not have the same problem because the toe is lifted. Because the toe does not yield to reduce the pressure, Zandra relies on cyclical podiatry to maintain comfort and prevent deeper damage in the form of a breakdown or ulcer.

Third-toe corn with a dark area associated with damage to capillaries in the skin layers
What is the puppet toe?

In writing this article on toes I wanted to tie up the concept of tendon overpull hence the name puppet. (Source) Here is a definition –
- An artificial figure representing a human being or an animal, manipulated by the hand, rods, wires, etc., as on a miniature stage. Compare hand puppet and marionette.
- A person, group, government, etc., whose actions are prompted and controlled by another or others.
- A small doll
Marionettes have strings or guides affecting their joints. Toes have tendons as guides influencing the joints of the toe. When learning anatomy in the dissection class, the toe moves into a different position if you pull on each tendon. Not all tendons are the same, and short tendons influence parts of the toe that long tendons don’t. The foot is a wonderful structure of mechanics.
The problem
Zandra wanted to know what to do with her toes. Her first toe having been operated on gave her no trouble, although the big toe had drifted slightly. Had she presented with her first and second toe together, the treatment plan would have been different.

The collection of devices used for protecting Zandra’s toe
Left to right. A traditional leather toe prop lies under the 2nd to 4 toes inclusively. It provides some lift and mild stretch to the flexor tendons. The pink mould is called Otoform. It is a siliconised wrap-around device that fits each patient’s toe as a gum. The mould sets within 2 minutes. The right-hand foam prop would have been made a temporary trial method, and like the leather, the device has toe loops. (WARNING – using these products is valuable for many patients, but the loop, if tight around a single toe, can cut off the circulation.)
- A primary regressing great toe position
- Multiple toe deformities each affecting different joints
- Transfer pressure (now alleviated by treatment seven years ago.
- Formation of an apical (end of the toe) corn with callus
- Formation of corn on top of the second toe PIPJ

Top (dorsal view). The first toe is seen drifting laterally, pushing against the second toe, which has lifted. The end of the third toe has disappeared in this view as it has flexed (mallet)
Facts of the matter
If most foot surgeons are truly objective, they would say a percentage of big toe operations work well; sources suggest failure can be as high as 50%. Some fail, and some cause a return drift of the deformity. In twenty studies reviewed by Migliorini, F, (2021), there was no mention of problems with hammer toes. The data used covered the period 1987-2018. One of the reasons why data misses out on evaluating failure is the limited follow-up period. Six – twelve months may appear reasonable, but changes continue within the first five years, and if truth be admitted, we often fail in our review process. Such failure can be explained by lack of funding, the process being too time-consuming and clinically inefficient (which is self-defeating, of course), and follow-up has a notorious dropout rate, with many people becoming untraceable through moving or lack of motivation. Quality follow-up and audit are essential to determine improvement and remove causes of failure.
However, even in a successful bunion correction, a patient might be pleased with the original results and have no further pain or symptoms but finds that the toe buckles and turns into that infamous hammer (claw) or even retracted toe. To the lay eye, this toe is buckled at the top joint A. The toe is lifted and affected at the next joint toward the foot. The alignment is out and shifts toward the big toe and is therefore dislocated slightly. In other words, the toe is out of alignment. If this toe is left, the skin changes over point A and will deteriorate.
The isolated second toe
Zandra’s second toe was dislocating mildly but not deviated. Untreated hallux valgus (bunion) deformities can cause this problem. The simplest approach is to straighten both the first and second toe together. If the toe problem arises later, as in Zandra’s case, we can deal with the toes alone. Evidence is poor, so we must look at the broader picture. Do we know when hammer toes start to be notable in the human population? Secondly, is this due to upset muscle mechanics or just acquired?
What is the incidence of this happening?
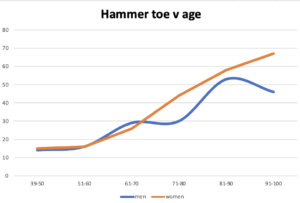
The graph shows females in orange with a line that increases more cleanly as age progresses. Men have a less distinct age-related curve (Golightly, 2014)
In a study conducted as part of the Johnston County Osteoarthritis Project (Golightly, 2014), 1466 subjects were described with hammer and claw toes. The majority of patients complain of hammer toes, as shown. Claw toes are often grouped with retracted toes, so they lift above the ground in many cases. Hammer and mallet toes tend not to do this; their tips often contact the ground or are only slightly raised. Zandra had a hammer toe, so the end contacted the ground, and her flexor tendon was tight as it had contracted over time. Golightly found a racial difference; the African American foot had a lower incidence of hammer or claw toes for all foot positions, and obesity, based on +30 BMI, had no difference compared to underweight subjects. The study implies that hammer toes creep with age and have no gender preference but are racially more prevalent in Caucasians. However, the Johnston project did not define how many toes were affected.
The toe is a puppet of tendon dysfunction
While evidence has been non-conclusive, in Part 2, I have uncovered some interesting information. The takeaway information comes from Takekawa, T. et al. 2022 who found that the tendon and muscle movements affected the flexion pull in the big toe and lesser toes in stroke patients. At the same time, this is a neurological concern and is based on the fact that two different long tendons, one from the big toe (FHL) and one from the lesser toes (FDL), can cause claw toe deformities to act together. We have always considered each tendon works differently but suppose the mechanics alter, as in the first toe, the lesser toes can alter their direction of pull. Takekawa considered using the paralysis agent Botox for the marked clawing effect to stop the toes from becoming overridden.
The proposal is that as the big toe becomes less efficient, which means it has less mobility, the second toe compensates and stabilises the foot by buckling. The third toe can then follow, and the fourth toe. As there are no specific studies published on the problem, we cannot validate this hypothesis. Perhaps as part of any preparation for surgery, we should inform patients that lesser toe problems might follow.
Because the index toe features more prominently, we see a hammer toe deformity existing alone. The foot does not have to be flat or high-arched, as recorded by Golightly (2014). This evidence could buck the theory that everyone believed the answer to toe deformity was related to flat or high-arched feet. When neutral feet were considered, the toe deformity was just as pronounced.
The Problems with surgery
If the second toe were fused (arthrodesis), it would rub against the big toe causing the skin to blister and form a corn or even an ulcer. If the toe were managed with a small piece of the joint taken away (arthroplasty), the toe would curve as it healed, forming a banana shape. Many patients don’t mind this but must be warned in advance of surgey. The toe settles down and is no longer bent. The other method, which is fiddly but works well enough, is to transfer the tendons.
Now, most readers do not need to know the details because transfers can be performed in many different ways. The principle approach lies in transferring a flexor tendon where it is detached and sewn into the top of the toe, so when the flexor contracts, the toe is pulled down without bending the joint.
For Zandra, the desire and objectives are simple. She does not want to have surgery unless it is essential. She would like a method of management she can apply herself. She also would not wish to have her first toe position revised.
Choices
Here is a brief rundown of options. A different approach may need to be considered if someone suffers from multiple smaller toe deformities. In some cases, that regressing bunion requires further surgery. Zandra has regular debridement of the two lesions on the second and third toe to keep her comfortable. Many patients are happy to use a podiatrist or foot health practitioner (UK) for this management and a digital device, of which some are illustrated.
- Select shoes with a soft upper without an inner lining. This allows her shoe to mould around the toe.
- She can wear sandals and open footwear in summer and in good weather to avoid pressure.
- If shoes with a shallow toe box are required, protection is helpful.
- Toes splints such as moulder silicone will only provide a splint but will not change the tendon beneficially.
- A gel or silicone sleeve available in line will protect the skin from rubbing, blistering, hard skin and corns.

Shoes stretching for unlined shoes can make a difference and can be bought for under £20 ($24)
Some surgical options for Zandra
- Simple tendon release where the flexor tendon is cut is useful, simple, quick and only needs a local anaesthetic. The length of benefit may be short, but even if this fails, no significant problem should have developed to prevent further treatment. This is only useful if the joint is not stiff and can be moved.
- A tendon transfer is one of the better options over arthroplasties. After an arthroplasty, the toe will mould to the big toe so it will be bent sideways, e.g. Zandra’s second toe. The corn would resolve. The MTPJ may need to be released as there is contraction present.
- An arthroplasty to Zandra’s third toe would completely resolve her apical corn. This can be undertaken without surgery on the second toe.
- Arthrodesis is not recommended, as a stiff toe against the big toe will lead to skin rubbing.
- Amputation is not recommended, although many patients do ask for this when there is significant pain or recurrent infection.
- Professional advice from a registered medically trained orthopaedic surgeon or a qualified podiatric surgeon is recommended.
If you have further questions, you may find the second part of assistance – Evidence helps to explain the problem – Part 2. This website also supports information on corns affected by hammer toes.
![]()
- Tollafield D R 2019 Bunion Hallux valgus. Behind the SCenes. A new foot pain series. Published Busypencilcase Communications. Available from Amazon books*
- Migliorini, F., Eschweiler, J., Tingart, M., & Maffulli, N. (2021). Revision surgeries for failed hallux valgus correction: A systematic review. The Surgeon (Edinburgh), 19(6), e497-e506. https://doi.org/10.1016/j.surge.2020.11.010
- Golightly YM, Hannan MT, Dufour AB, Hillstrom HJ, Jordan JM. Foot Disorders Associated With Overpronated and Oversupinated Foot Function: The Johnston County Osteoarthritis Project. Foot & Ankle International. 2014;35(11):1159-1165. doi:10.1177/1071100714543907
- Takekawa, T., Takagi, S., Kitajima, T., Sato, T., Kinoshita, K., & Abo, M. (2022). Claw Toe: Anatomic Guide for Injection of Botulinum Toxin into Foot Muscles. Canadian Journal of Neurological Sciences / Journal Canadien Des Sciences Neurologiques, 49(1), 102-108. doi:10.1017/cjn.2021.52
* Amazon book purchase of the bunion book is available direct from the author Amazon price £18.99 + PP. For (UK, including Northern Ireland) CFP readers – £15.00 + PP direct. Contact David at busypencilcasecfp@gmail.com to arrange delivery and purchase.
Thanks for reading ‘A Puppet Toe’ by David R Tollafield. Acknowledgement to Zandra for sharing this information with CFP. Don’t forget to read Part 2

Published by Busypencilcase Communications Est. 2014 for ConsultingFootPain

Recent Comments