Unravelling a Confusing Pain in the Foot
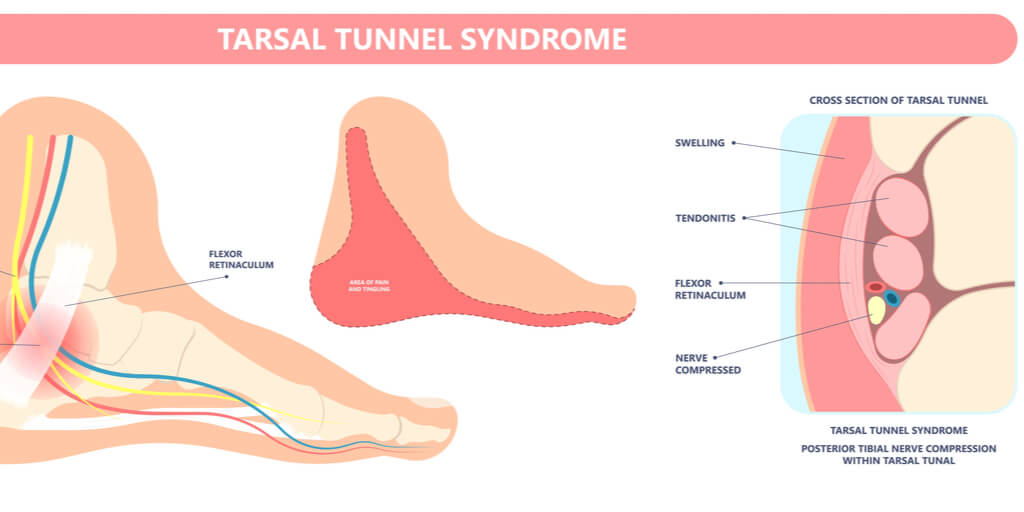
I want to introduce you to the condition called tarsal tunnel syndrome, which is a cause of heel pain but with the distinctive quality of the pain burning. The second feature that gives the condition away is that feeling of fullness, a sort of exploding sensation when exercising, worsening with standing, walking or running. Sometimes, this type of problem pain is called referred. This means that the source of pain and location may not match. The pain may be in front of the foot but is related to the structures in the hind part of the foot. When reading this article, there are some useful sites I have used that you can select by clicking on blue headings, i.e. Factsheets and Advice.
Why is it Called a Tunnel Syndrome?
A syndrome is usually applied to a condition where the problem is associated with another disease entity. This means that a condition known as plantar fasciitis or tendon pain can become involved with tarsal tunnel pain problems. The diagram illustrates the tunnel under the ligament (green).
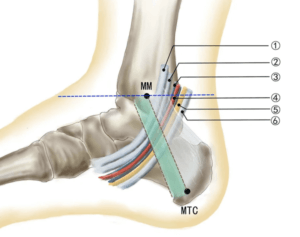
MM: medial malleolus. MTC: medial tubercle of the calcaneal. The blue horizontal line is Line A, which crosses the tip of the medial malleolus. The green oblique line (band) is Line B, with a 1 cm width, which spans from the tip of the medial malleolus to the medial tubercle of the calcaneus. This axis also represents the inferior edge of the flexor retinaculum and, consequently, the tarsal tunnel. ① Posterior tibial tendon, ② flexor digitorum longus tendon, ③posterior tibial artery, ④ vein accompanying the artery, ⑤ posterior tibial nerve, ⑥ flexor hallucis tendon. C/O Yang, Y., Du, M., Fu, Y. et al. Fine dissection of the tarsal tunnel in 60 cases. Sci Rep7, 46351 (2017). https://doi.org/10.1038/srep46351
*****
Problems with the tarsal tunnel have similarities with the carpal tunnel in the hand. The green band is a ligament and very much simplified, but it serves the purpose of suggesting something tight crosses over the motorway of blood vessels and tendons. The yellow line is the tibial nerve, which is the thickest part of the foot. As road branches, so do nerves and blood vessels. As the tibial nerve passes forward, it curves under the foot, but before this, it sends higher branches out. If the nerve is compressed, damaged or has fluid within the tunnel, then the nerve will not conduct correctly.
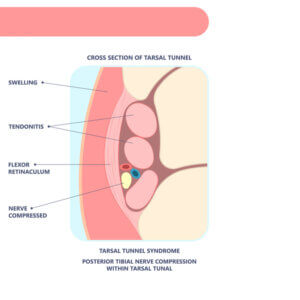
The arrangement of the tendons, blood vessels and nerves is clearer in this picture.
Inflammation is a process where fluids increase (oedema), and this alone can cause a problem. The fascia makes up part of the arch of the foot, passes close to the tunnel, and can influence pressure. If this happens we advise clinically managing the fascial pain. Once fluid reduces, the nerve should return to normal. Life becomes complicated if the tendons are swollen because they have to be relieved of pressure and pain. Shin splints are often labelled due to tendon overpull. If the lining tears, the tendon sheath effectively leaks, causing more pressure. True tarsal tunnel syndrome (TTS), therefore, does not have one but may have several causes. Unlike the hand, the last thing you want is someone opening up the foot. Well, that would be unless the nerve has a growth on it or the nerve itself clearly is swamped with a fluid that needs releasing.
Compartment syndrome is another condition in which fluid builds up and affects groups of muscles constrained under pressure. It is different from TTS and threatens the blood supply. Increasing pain does need to be investigated, particularly if it worsens during exercise, but TTS does not usually involve a severe blood supply deficit.
Diagnosis
Tarsal Tunnel Syndrome (TTS) is both complex and can resist treatment. Achieving a diagnosis is not difficult; it commences with taking a history and identifying the length of symptoms and when they arise. A simple test is called a Tinel sign where the nerve around the inside ankle is tapped (percussed). The video shows a reflex hammer, but finger-tapping works as well. Valleix is another sign where, after tapping, the signal travels in two directions. Radiating tingling (paraesthesiae) suggests the chance of some restricting of the nerve, which includes scarring. The tibial nerve is around 3-5mm thick and very visible at operation.
Veins can become engorged around the nerve and can produce similar symptoms of tingling and burning. The typical imaging tests are ultrasound and MRI, but early signs are not easy to spot. A useful test is to inflate a pressure cuff around the ankle and compare the two limbs and the respective responses. Discomforts below 100 mmHg (pressure) should be considered worth following, especially if tingling is noted. Once the pressure drops below 70mmHg to inflict notable symptoms, then it is reasonable to seek further imaging. Patients should usually tolerate 120mmHg unless the limb is impoverished or has any associated rheumatological condition. Nerve conduction tests play a role in measuring the speed of nerve signals. Slow values suggest obstruction.
One of the difficult problems facing a foot specialist is that a neuroma between the toes (Morton’s neuroma) can produce similar pain in the forefoot. It is possible to have TTS and MN together, so both must be managed separately.
Burning pain is unpleasant and sometimes called causalgia.
Different levels of discomfort
Pain means different things to different people. Gender, genetics, and age all contribute to different patterns in how we cope. The impact that pain imposes on humans is associated with the effect of pain on daily life. Pain affects sleep and emotions. Signs are different from symptoms. Accurate description affords more transparent communication. To help, a scale allows pain to be rated from none to worst, with 0-10 being the most popular. A diary provides better consultation with healthcare professionals. Diaries may take different forms: charts, electronic diaries (spreadsheets), calendar style, or formal descriptive styles.
Timelines are important for charting the origin of the problem. It becomes obvious that the longer pain is sustained, the more damage occurs and the more difficult it is to reverse the condition. Referred pain may come from nerves elsewhere or alter posture from the original site in the foot. Burning (causalgia) pain should not be allowed to become chronic.
Treatment
The use of medication for pain broadly includes medications such as paracetamol (non-anti-inflammatory), aspirin or ibuprofen (anti-inflammatory), and codeine. Drugs have to be used responsibly but only for 2-5 days before one should seek help. The idea is to identify pain that can be improved. Where medication fails, professional assistance is required because nerve compression may respond poorly. When approaching a professional such as a GP, it is useful to have some prior knowledge of the condition because many practices will allocate urgency through telecommunication. Having a pain diary to hand is helpful.
True TTS requires support from professionals and early signs of numbness in the toes, the fullness of the forefoot, or pain during activity are your key indicators. Bear in mind that this is a syndrome, and so if you have plantar fasciitis, you can go down the stretching route. Pain is easily identified as it has pain points in the heel. If it has to do with the tendon, you can feel discomfort, such as deep aching behind the inside ankle bone. Ice can help with extreme cases or local gels such as voltarol or ibulieve. My article on shin splints and tendon dysfunction provides some self-help tips.

Check for tendon pain – dull aching on activity, which continues at rest
What can be done?
General information on this condition can be accessed from a number of useful sites, such as FootEducation (2017), and divided into non-surgery and surgical choices. The following article from the Marathon Training Academy (Ben Shatto 2018) might be helpful to and covers other conditions associated with this condition. Bear in mind that if too many months have passed without intervention and the condition progresses – self-help methods may well be disappointing. Use my tips on dealing with Morton’s neuroma.
As far as self-help is concerned –
- act early
- check shoes
- find what makes the pain worse and take action to prevent any further irritation
- consider orthoses for poor foot alignment – orthotic care
- decide if this is plantar fasciitis, tendon pain (posterior shin splints)
- Tap around the ankle (Tinel’s sign). If the nerve sends tingling to the toes, then hold a suspicion you may have TTS and seek help early
- Is this Morton’s neuroma – localised toe tingling
- surgery is used only in cases where pain does not subside
Those wishing to know more about TTS surgery should use the FootEducation link. Open surgery is used, and some surgeons use minimal surgery with optical scopes. Seek professional advice from a podiatric surgeon or dedicated orthopaedic foot surgeon.
Consider this introductory book to the adult foot, available from Amazon or from the Institute of Podiatrists.
An Introduction to the Foot & its Common Problems in the Adult.
Published by Busypencilcase Communications Est. 2015 for ConsultingFootPain


Recent Comments