A Twenty-Eight Year Follow-Up
A Patient Conversation
While many published articles cite cases followed from one to five years this is probably insufficient to assess the longevity of correction. While foot surgeons try to select the best procedure and maintain a healthy joint, deformities can reoccur. Identifying an absolute cause is not easy, as scientific controls are complicated, given many variations called confounding factors.
We do know that surgery on young feet has a high chance of further deformity and is best left until later in life. In this next case study (2024—edited), a respondent wrote.
Patient J:
My hallux valgus was operated on at thirty-five. A wedge was removed from the first metatarsal, and the big toe had a pin insertion (Fig.4.8), marked as screw fixation. The surgery was very successful, both in terms of aesthetics and in resolving foot pain. I was able to get back to work as a pharmacist on my feet all day. Unfortunately, twenty-eight years on, I can see no alternative but to have a further procedure, as the condition has gradually reoccurred – and to an even greater extent now, with the big toe crossing over the second toe. This will undoubtedly cause balance problems as the big toe is not properly in contact with the floor, not to mention my embarrassment over the appearance of my foot and difficulty with footwear.
Aside from the post-operative discomfort and downtime and wanting to avoid a general anaesthetic, I also have concerns about finding a surgeon/hospital as my late Mum had a hallux valgus operated on by a surgeon at X Hospital, with a completely unsuccessful outcome.
As an expert in the field, I would like to know if you could advise me on how best to proceed. Would you have any pointers on the optimum technique/procedure to correct this (including any information on ‘minimally invasive’ procedures?)? Certainly, any knowledge of suitably experienced surgeons would be greatly appreciated. I only wish you were still operating!
Response:
Twenty-eight years is typically around the active lifespan of a surgeon[1]. Consult a dedicated foot surgeon, either a Fellow of the Royal College of Surgeons (FRCS) or from the Royal College of Podiatry (FRCPodS).
The base wedge osteotomy does cause a small amount of shortening (Fig.4.8.), so your most reliable, longer-term solution is to consider a joint fusion (arthrodesis).
The arthrodesis procedure stiffens the toe and sets for a specific heel height. Arthrodesis is regarded as the gold standard for revision work. The recurrence is unlikely and should last until the end of life, but most of us do not perform this as a first-line surgery as younger people prefer to opt for toe movement.
Select surgeons whose primary practice is foot surgery. Dedicated orthopaedic and podiatric surgeons are good at what they do, but experience in revision surgery is essential.
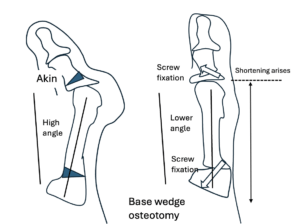
Fig.4.8.The base wedge osteotomy is favoured less as a first-line treatment. It is useful for large deformity angles but should be avoided if the first metatarsal bone length is initially short. The bone shortens in this procedure and allows good joint movement, but it can take up to a year or more to achieve this.
The case is based around one type of operation and does not necessarily hold true for all operations, but many cases do require revision where symptoms arise.
Patient J:
My initial instinct is that it seems counter-intuitive to fuse a joint with no current stiffness or pain, and if the toe ends above the floor, it may not improve the balance issues. However, it makes sense that it would prevent the reoccurrence of the hallux valgus. I would like to hear your thoughts on minimally invasive surgery, if it is relevant to my situation.
Response:
Revision surgery comes with heightened risks of failure and complications. The shortening of the bone is the most relevant. Long-term studies on bunion surgery need to meet scientific standards; a 30-year follow-up is unavailable. Revision surgery after several years after primary surgery can be successful.
Fusion is a safer bet than most alternatives and offers better longevity. Third surgeries seldom come without loss of function. More surgery involves deeper tissue scarring, and even then, a joint-sparing operation could lead to limited joint movement. Minimal incisional surgery (MIS) appeals to many for obvious reasons, but the follow-up is not as well presented as other surgeries and is limited to specific criteria. MIS is available and has advantages. New screw systems allow surgical placement through keyholes under X-ray-guided control.
Do not overburden the second surgeon with annoyance or disappointment with the first surgery. You cannot expect the second person to react in the way you wish they would respond to a colleague. You’ll find that medicine is inevitably protective and cautious where everyone feels under scrutiny, perhaps more so today than ever before, with a high level of litigation. Avoid making statements advising on litigation or making any statement that claims negligence against the first surgeon.
[1] This case was author DRT. Taken from A Complete Patient Guide for Bunion Problems. Published January 2025 and now available from Amazon books as an ebook, paperback and hardback.
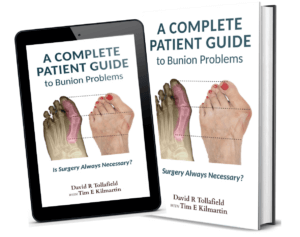
This is one of the most detailed books available today, written by two consultant podiatric surgeons with sixty years of experience between them.
My family doctor says he doesn’t know the answers to my questions, and I don’t want to make another mistake or have fusion if my feet can be fixed. I really value your opinion, and I have not been so fortunate to find someone here like you that puts out so much helpful information for everyone and answers questions and comments at the end of articles—Gail —a desperate patient.
Although I’m used to approaching everything from a textbook point of view, the patient’s perspective revealed that there’s much more to decision-making than just focusing solely on the clinical and anatomical causes for action. It wasn’t structured like a textbook but provided the same depth of knowledge, but it was much more enjoyable to read and easier to understand—Sahiba Atwal—Final Year Podiatry Student, University of Southampton.
Thanks for reading ‘How Long Does Bunion Surgery Last?’ by David R. Tollafield.
David is a full-time author and blogger working with Busypencilcase Communications & Publishing. Est. 2015.

I don’t see how a suggestion of joint fusion (or any other procedure) could be given without X-ray first
I am sure that a competent surgeon would need to review the bone quality and joint before executing any surgery. It all comes down to a balance of details between how much information one should offer.