Sub-Ungual Exostosis
Causes of painful toe swelling
Curious shapes, distortions and nail problems are always fascinating to podiatrists. The distortion of the end of the toe and callus formation in some of my patients was not uncommon, and I had to treat this together with what we call the nail apparatus. The term collectively involves the nail bed. A red, hard swelling was evident in young patients, usually under 30 years of age, where the nail was often thin and heavily distorted.
If it looks suspicious, it probably is not right, but that doesn’t mean it’s malignant!
Exostosis is an abnormal outgrowth of bone, while sub (under) and ungual imply the tip of the toe. Ungulates such as horses walk on the tips of their toes and their nails have adapted into a single bone and toenail, the keratinised hoof.
There is a dearth of material from some of the formal UK sites, but the NHS and Wye Valley NHS Trust have written a specific guide sheet available to download here (guide sheet) checked 23/1/25. When it comes to factsheets and guides, one certainly finds great variations, and there is no doubt if you perform a search, you will find more information, often from the USA. Bristow’s article and Dermatology Advisor are valuable.
What is it, and why is it confusing?
The condition seems to be limited to the young because of immature cells being involved. We know that chondrocytes can change to osteocytes as part of growth development, and chondrocytes are the name given to cartilage cells. This is the soft material that you find on the ends of bone joints with raw meat and chickens.
An injury to the toe is common, not least because the toe sticks out at the end of the body. The excessive growth, like hyper granulation in an ingrown toenail, confuses the clinician because the skin is shiny, stretched, red and easily knocked. I always sent off my bone samples once removed at our local hospital for some years, and they used a specialist hospital in Glasgow to peer review any interpretation. I knew that elsewhere in the body, the bone-cartilage lesion known as an osteochondroma could become malignant in <5% of cases, but in the foot, this is rare.
My youngest patient was 10 years old, and the average patient was probably around 19-20, with the oldest osteochondroma at 35 years. I have seen pseudo exostoses, little spikes in all ages, but the subungual osteochondroma forms thickened skin that looks odd, as it has blood vessels running through. This can be confused with angiokeratomata. These are defined in an article by the Primary Care Dermatology Society (PCDS).
Again, the skin with its blood vessel distortion and raised nail edge can be caused by the end of the toe bone sticking out with cartilage capping over the end (see Figure 1 below), where the skin is stretched. Illustration A shows the nail-distorting type of exostosis, or subungual projection, distorting the nail, while B shows the smaller phalanx of a lesser toe projecting abnormally forward. The red areas indicate stretched skin, and in the case of A, the nail may appear soft, thin and moulded.
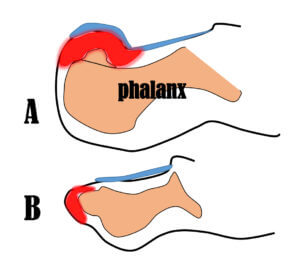
Figure 1. Two scenarios. Subungual exostoses are often associated with osteochondroma. Nail in blue. Skin stretch red. Bone pinky-orange
Planning & Treatment
Radiology is mandatory. Resist the ever-increasing passion for debridement, as the skin will bleed easily. A healthy suspicion of cartilage must be considered in younger age groups. A biopsy (sample specimen) is not needed if surgery is being performed, as radical excision (cutting out) is necessary, with nail bed repair afterwards.
More often, the nail returns only slightly damaged after surgery, but all patients must be made aware that the nail may be permanently thickened, discoloured, or distorted. Permanent removal can deal with this later. Guide sheets, such as the one produced by the Wye Valley podiatric surgery department, will inform patients what to expect and how to best recover after surgery.
- For the patient, any swelling should be examined by a professional if it is slow-growing and no notable injury is attributed.
- Wear open-toed footwear until you can see someone or as deep-toe boxed shoes as possible. Soft uppers might be better to avoid pressure.
- For the podiatrist or GP. Take an x-ray if suspicious and act upon the findings.
- The lesions are rarely malignant but should be treated with moderate urgency to seek an early diagnosis from an excisional biopsy.
- All surgical treatments should come with a fact sheet and post-operative guide.
- Surgery is suited to local anaesthetic management in appropriate facilities.
- Histology is always advised with this osteochondral lesion, but such decisions will be based on the surgeon’s experience and local policy.
Should any other specialists see a patient? This will depend on your local area; those who have appropriate training and experience in foot surgery are the people to discuss treatment with. If in doubt, speak to your GP as to who to see in your area, but it is essential to make it clear that you are trying to rule out malignancy, and delay should be avoided. After the effects of COVID-19, it is difficult to predict the speed of referrals onward, but a direct referral to a specialist is much preferred, and this is where a quality referral letter is required.

You can read more about feet in David’s book, which covers an introduction to feet popular among lay readers and students.
David is the principal author of ConsultingFootPain and retired from clinical practice in 2018, becoming a professional writer. Click below to see his latest books. He specialises in writing for the lay public.
Thanks for reading ‘A Bone Swelling on the Big Toe’ by David R. Tollafield.
Produced for ConsultingFootPain by Busypencilcase Communications. Est. 2015


Recent Comments