Shingles & the Dorsal Root Ganglia
Sensitivity and Causalgia
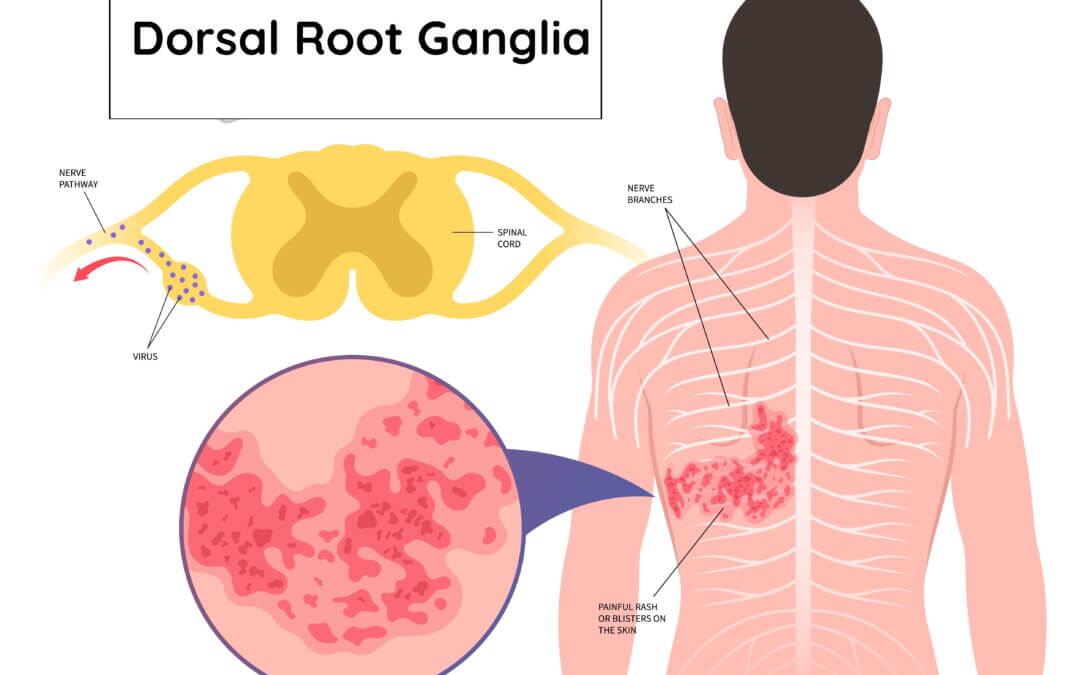
Shingles can appear anywhere from the head, arms, chest, abdomen, or buttocks to the feet. I have never seen feet affected, and the buttocks were not mentioned as frequently as the upper girdle and lower back. However, it is the dorsal root ganglion DRG where the virus sits, just waiting for the right conditions to come along and strike. Why a virus that is related to chicken pox does this is not clear. The DRG seems to be a car park for special nerves.
Shingles is such a bad condition because of the lingering effects of postherpetic neuralgia. This hypersensitivity creates a different type of pain when the slightest touch or brush of clothing irritates the nerve endings. The second sensation is attributed to this viral condition, which causes burning or causalgia symptoms, but the DRG is an amplifier for nerve endings.
The risk of avoiding protection
I am interested in the dorsal root ganglion (DRG) because, for over thirty years, I have been involved in the clinical condition of complex regional pain syndrome. Faced with the burning pain associated with shingles, I was now in a prime position to relate to the symptoms that some of my patients experienced.
My wife was offered the vaccine in December 2021, as she satisfied the criteria. However, she decided to put it off until she returned from her holiday because she knew the vaccine could potentially cause shingles. One always has to balance the risk, and the holiday was in the Caribbean, so if she had reacted, the holiday would have been off. Now we were at the end of 2024 and Christmas with the family, and I was struck down. This raised the question of Controversy over who was entitled to the vaccination. You can read the story of Shingle Bells here.
What is a Dorsal Root Ganglia (DRG)?
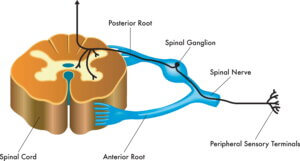
Medical illustration showing the connection of the spinal ganglion to the spinal cord, with annotations regarding the pathway.
The spine is an extensive motorway with two-way traffic. It is licensed to carry different nerves down this motorway that cause sensation (sensory) and muscle movement (motor). This article focuses on the sensory nerves, but we must also recognise that other nerves are more automatic and do the heavy lifting, controlling our organs. The illustration shows the central spinal cord, which goes from the brain stem to the tail end or coccyx area. Once it reaches this latter point, the nerves no longer have the vertebral bones to protect them.
Just like the junctions of the motorway, nerves branch off to supply everything from muscles to skin and organs. In the upper body (trunk), upper arms and legs all have different roots supplying them, and in most cases, more than one. The illustrations below show the distinctive pathways, but the sensory pathway has a bulbous section outside the spine. This is repeated along every segment or junction. The Seladi-Schulman (2024) illustration shows dermatomes, which are areas of skin supplied by nerves.
This bulbous area, called the dorsal or posterior root ganglia (DRG), is located in the back. It is packed with spinal sensory nerves and registers chronic pain. A DRG arises at each spinal level, from the neck to the sacral (buttock) region.
The system transmits signals from the exterior to the brain. Specialised nerves are linked to pain, and certain chemicals can heighten the sensation of nerve (neuropathic) pain and inflammation. As indicated by the name, neuropathic pain is related to the nervous system. Still, the distinction lies in the type of pain— characterized by a burning sensation and an exaggerated sensitivity that can intensify with the lightest touch. For instance, the friction of clothing can be unbearable. Furthermore, the nerve fibres can send error signals, causing pain to radiate to the limbs.
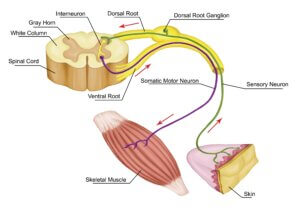
The nervous system shows the nerve supply to muscles and skin.
The long-term effect of the nerves within the DRG failing to settle after being affected causes skin blisters at the end of those nerves where the DRG becomes active. As the blisters either burst or crust over, the itching and burning sensation settles slowly but still leaves a sensitivity. If the sensitivity continues, despite the skin rash and blisters no longer being visible, the condition becomes both chronic and complex.
The virus also infects the nerves associated with the brain (cranium) and again has specific branches. The trigeminal nerve may be affected, putting the eye at risk of blindness. T

Blisters remain a typical sign of shingles on one side of the body. Cranial nerve infection can lead to blindness.
The question remains: Why do shingles lie dormant for maybe fifty years, and why focus on the DRG?
In my case, symptoms affected above the groin (lesion), and hypersensitivity ran down the inside of my leg. The lumbar and sciatic nerves were affected. Seladi-Schulman (2024).
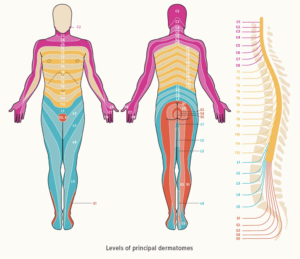
Courtesy of Seladi-Schulman (2024) Dermatomes
The virus affects specific areas of skin linked to the nerves pertinent to the DRG in question. Each spinal nerve corresponds to an area of skin, and in my case, the buttocks are supplied by the sacral branch, specifically S2-4. These correspond to dermatomes, meaning that for thirty-one spinal nerves, there are thirty dermatomes, although each dermatome can vary from person to person. A shingles rash forms along one or two dermatomes on one side of your body, with its location determined by which nerve the virus proliferates from. The rash does not cross the midline of your body because each spinal nerve provides sensory information solely for either the left or right side of your body. (Seladi-Schulman 2024).
Conclusion
Shingles (Varicella-Zoster) lie dormant, affecting more than the dorsal root ganglia. There is no substantive reason why it focuses at this point, except it is in an available car park of neurons dedicated to gathering information and reacting to stimuli. The DRG makes the location and opportunity out of susceptibility. This means when the immune system is lowered, the virus cannot be contained as it was when young. Post-herpetic neuralgia does not affect everyone, but depending upon which dermatomes are affected and the location of the blisters, the inconvenience is undoubtedly likely to remain for one month or more.
Thanks for reading ‘Pain and the Dorsal Root Ganglia’ by David R Tollafield
Don’t forget to read my personal experience of shingles here.
David is a blogger, author, and former consultant podiatric surgeon who writes for ConsultingFootPain under Busypencilcase Communications, established in 2015. His sub-clinical interests have been rheumatology, pain neurology and pathology. He has written several books as guides for patients, comparing his own experiences with medical health. His latest book is A Complete Patient’s Guide for Bunion Problems.


Recent Comments