Different Ideas of Pain
Differentiating between acute and chronic pain becomes important, not just for feet but for pain anywhere in the body. In this article, I will discuss pain medication and its meaning. Developing a self-help strategy and knowing when to seek professional help is also essential.
The information in this article is more general and should help inform lay readers of medication and other methods to deal with pain. The subject of acute and chronic pain is massive, with much ongoing research by a number of medical and scientific bodies. While medication is helpful, we must try other methods to avoid medication dependency. You can read Part 1 on medication for foot problems (click here), with a special section highlighting addiction.
Acute pain
Infections
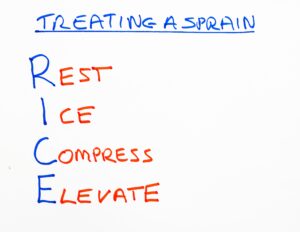
Infections need to be assessed for damage and spread. Pain medication helps but does not cure the problem. First aid should also be attempted by cleaning wounds, applying antiseptic and providing a dressing. The dressing prevents further infection and absorbs discharge. Ankle sprains should be rested initially (self-help for sprains). Ice is helpful to pull down inflammation. NSAID medication works well here. Use a stick or crutch, if available, to reduce putting excess weight through your foot.
Joint pain
Ibuprofen for joint pain in the form of gout can work well but may need other medication. This is an acute problem. Constant pain and reoccurrence may require medication that prevents the joint from having repetitive flare-ups. In the case of other joint pain, rest, ice, elevation, and avoiding excessive activity will minimise pain and help heal. A swollen joint that does not reduce within 48 hours, causing increased disability and resisting pain medication, needs further advice.
Chronic pain
Chronic pain is perhaps far more common than we think and affects us all, especially as we age. Chronic pain lasts and is continuous. The body becomes resilient in coping, but the nature of chronic pain can be disabling. The problem between acute and chronic pain is that the acute form might settle. Chronic pain, on the other hand, may come and go. Old injuries that have left damage can flare up with overexercising.
Arthritis may flare up from day to day, season to season. Inflammation can become sub-acute, fitting between acute and chronic. The picture can become confusing. Pain clinics in the UK are inundated with chronic pain referrals and can barely manage them. I have included a link to a help site that deals with the worst type of pain—called Burning Nights. The cost of chronic pain to the nation is staggering.
Approximately 8 million adults in the UK report chronic pain that is moderate to severely disabling[1]. Back pain alone accounts for 40% of sickness absence in the NHS[2] and overall it costs £10 billion for the UK economy[3]. The UK has some of the best pain services in the world and the multidisciplinary British Pain Society is at the forefront of informing the public and professionals of what is available. 7 March 2018
Upsetting the stomach
Medication can upset our bodies, and no person is the same. This means we cannot all share medication. The stomach and bowels are the chief targets for the upset. You might have loose stools or become constipated. However, a rash might occur from sensitivity.
The first side effect is common and should settle when you cease taking the medication. This is NOT an allergy. The second could be an allergy and a side effect from taking the medicine. The trouble is that we do not know who is sensitive until they have used the medicine. Younger people are more at risk from the unknown of medicines where they have never used them before. It is essential to realise that some over-the-counter medications have ingredients that can interact with some medicines, such as simple cough medicines.

Follow the pharmacist’s advice and also share your knowledge of other medicines you are using, whether prescribed or self-acquired, especially if you are feeling unwell.
Pain as a Traffic Light
Pain is the body’s signal that something is wrong, but hopefully, it is only temporary. It is important to target the pain with the right approach. Do you need pain medication? Can you cope? Are there other methods you can use?
 Alternative methods of self-help
Alternative methods of self-help
Acute injury causes greater swelling than chronic inflammation, so rest, ice, compression, and elevation are best. This is often known as RICE. An example is ankle sprains. This approach can calm nerves and prevent movement. Anything that slows down the release of chemicals causing inflammation is helpful. Gels, creams, and ointments applied externally can be helpful, but they are probably more effective when used with medicines taken by mouth.
Natural methods
Some natural medicines, foods or herbs have helped with pain management. These include cloves, turmeric and arnica. Willow bark is also included but has some of the natural salicylate ingredients in aspirin. However, natural painkillers may only be effective for specific causes of pain. Not all suggestions will work for you. If you are sensitive to a medication, you might think about alternatives. Please refer to natural resources and specialist help if you prefer natural or homoeopathic medication. Homeopathy is never far from controversy and is under review by the medical professions.
Scaling Pain 0 (none) – 10 (worst)
Some scales measure 0-100, others 0-10 or 0-5. If you scale at 1, ‘RICE’ may be the only thing required, but scaling at 2-4 will benefit from better pain management + RICE. At 4-5 pain level, you may need professional help. As with all scales, this only acts as a guide.
The Pain ladder
Clinically, we talk about the pain ladder so that if you score at levels 2-4, you will need something effective. Acute pain may settle fairly quickly. By using pain medication, you can soon tell if the problem starts to improve. If it doesn’t improve, then seek help. The timescale may be from 12 to 48 hours. If unsure, you can always contact 111 for free professional advice outside of office hours in the UK.
Chronic pain is a different matter, and we want to control it. Pain from a sudden injury is acute. Chronic pain comes from overworked muscles, joints, and tendons. Poor healing will also result in chronic pain. Nerve pain falls into both camps and depends on what is happening deeper down.
‘That stuff the pharmacist gave me didn’t touch the spot!’
Know what works for you and what you can tolerate, and don’t share medicines.
Where to start with analgesics
Paracetamol 500mg can be used up to 8 tablets in 24 hours for a good reason. This type of medication will deal with most pain as long as it isn’t 4+. Increasing your control by adding 200mg of ibuprofen for short periods is permissible to overcome the acute effect. Do read the advice on the box. Some over-the-counter or sales products include the two medications – mixed. These are known as compound medications. If your pain escalates, you should not start doubling up. Liver damage is non-reversible and terminal. Two tablets are sufficient and spaced over 4 hours. So, 2 every 4 hours is usually directed on the packet.
Ibuprofen is often branded as NurofenTM in the UK and sold in 200mg or 400mg strengths. Unbranded forms are cheaper. The higher dose is for convenience, as most directions suggest two tablets every 6 hours at 200mg strength. One tablet can, therefore, be taken every 6 hours at 400mg strength. This medication needs to be taken after food. The ingredients can cause stomach (gastric) irritation and feeling sick.
Top of the self-help ladder
When pain worsens, it is possible to add another over-the-counter medicine, which is codeine. Codeine, however, now comes with much greater concerns than previously thought, and it may be re-regulated in time. A mild derivative of the opiate (morphine), codeine can become addictive. Addiction can creep up on you without noticing, even in small doses. The more medicine you use, the less effective it becomes because the dose needs to increase as you hit a threshold value of effectiveness. Currently, codeine is generally mixed with paracetamol or ibuprofen. The non-prescription doses are low at around 8mg. Even low doses of codeine can produce constipation because it lowers the effect of muscles on bowel movement.
Always Read the Leaflet
All these medicines work for pain, but aspirin and ibuprofen also work for inflammation and swelling. These last two medicines should not be used with gastric ulcers or inflammatory bowel problems and can interact with blood thinners (anticoagulants). This list is not exhaustive, and reading the leaflet with tablets is important as it will cover other concerns.
Side effects
Codeine: Those who have never used this medicine (drug) may find they become woozy, spaced out, and disoriented. This is not a pleasant sensation, so it is best taken when resting. www.nhs.uk is a useful site for information on most health issues, providing safety information and advice.
What form of medicine
 Tablets can be capsules. These may be slow-release so that the pain relief factor is slower but more gentle and lasts longer. A dispersible format comes as a larger tablet that fizzes when dropped in water to become a solution. Soluble tablets act faster as there is no coating, and in solution, they offer a larger volume of the active ingredient.
Tablets can be capsules. These may be slow-release so that the pain relief factor is slower but more gentle and lasts longer. A dispersible format comes as a larger tablet that fizzes when dropped in water to become a solution. Soluble tablets act faster as there is no coating, and in solution, they offer a larger volume of the active ingredient.
Alternative forms
Ibuprofen is a non-steroidal anti-inflammatory (NSAID) medication that comes in as a gel and ideally acts faster. It helps relieve pain around joints and muscles and is for soft tissue pain. Hard tissue is bone. There are plenty of alternatives now: Emugel (diclofenac cream), Movelat (Mucopolysaccharide polysulphate with salicylic acid) and Feldene (piroxicam) gel. Sensitivities can occur, and some cross over with aspirin. If you are sensitive to aspirin, then you may be sensitive to Feldene or another NSAID.
You should not spread gels and creams over large areas because these products absorb into the bloodstream and can irritate the skin. Gels and creams are helpful for mild pains and aches.
NICE, the national body for evidence and safety in the UK, is reviewing the overuse of painkillers for chronic pain can cause problems.
Summary of Points
- Always read the packet and instructions first.
- Do not exceed the dose stated.
- Be aware of allergies and sensitivities.
- If you have stomach or other problems, seek medical advice before use.
- Don’t mix the medicines with others you take. Discuss with the pharmacist.
- Codeine products containing paracetamol should not be mixed with separate paracetamol.
- Take the most effective medicine early at the top dose recommended for acute pain.
- Use pain medication together with the principles of RICE
- If pain is not managed (worsens) after 3 days, seek professional help, or seek help if you feel unwell or have a high temperature.
- Gels and creams should not be used on open or infected wounds
- Avoid addiction recognised by overuse of medicine without medical direction
David is a full-time author, blogger and independent publisher of health matters and fictional works. You can find more about him on this site or his author website. Please share this article.
You can read the story of Anna Taylor in Fatal Contracts and the Withered Hand, released in August 2024 – from Amazon books in eBook and paperback under his pseudonym RC Blyth . You can also follow David on Facebook @davidtollafild, LinkedIn and X @myfootjourneys.
Thanks for reading the second of my two-part article. ‘Acute and Chronic Pain’ by David R. Tollafield.
Published by Busypencilcase Communications & Publications
Established 2015
for ConsultingFootPain
Published 1 February 2021. Modified January 2025

Recent Comments