Is back history just padding?
Foot neuroma is often called Morton’s neuroma when in fact it isn’t. Most modern papers commence with the background history. Is this valuable or just padding when writing papers? So we meet the inevitable older problem, that is, who initiated a treatment or described a condition? Perhaps we do need to go back?
Keywords: PDN plantar digital neuroma. MTPJ metatarsophalangeal joint
Plantar Digital neuritis
Take ‘Morton’s neuroma’, known officially as plantar digital (neuritis) neuroma (PDN). Morton’s neuroma is an old problem that there can be no question about. More has been written about this than many other foot entities. When I found out I was suffering from the same condition as my patients, this metatarsalgia required new analysis. I say metatarsalgia because this forms a group of conditions causing the ball of the foot pain or metatarsal pain. I felt it important to combine all three skills – patient, podiatric surgeon and author, to reveal some unknown aspects. Many textbooks dedicate a small section to this condition. To be able to read and dissect all that is published creates a mammoth task for any clinician. One of the fastest methods to achieve any type of assay on published clinical papers is to go to those written as a meta-analysis. Even with this resource, some references must seek out the original references, so I must start.
Back history and padding explained
In the case of PDN, papers talk about Thomas George Morton, who wrote about pain around the fourth metatarsophalangeal joint (MTPJ) rather than an interspace between the third and fourth joints (third space) in 1876 (CORR 1979). Moreover, his original paper presents 12 case histories.
The Italian Filipio Civinini was an anatomist and during dissection, he came upon what he described as a ‘neural ganglion swelling on the sole’ in 1835 (Arauz, 2020). However, his name is associated more frequently with other anatomical features, especially the cranium. Morton’s original paper was concerned with the 4th MTP articulation rather than nerve pain. As such he applied crude surgery far removed from minimal surgical incisions of today or guided injection therapies.
Accidents provoke learning
During one of my theatre sessions, a patient scheduled for a single digital amputation back in 1997 caused some alarm when I noticed a large butter bean-sized pearly glistening tissue. It was clear that her 2nd-3rd interspace had a massive neuroma – the only problem was that her toe was half off!
This seems unforgivable now, but we had no ultrasound, and MRI was not the first line. Nevertheless, there is some correlation with Civinini’s experience here. It might not surprise that some papers call PDN Civinini-Morton’s neuroma. While the Italian anatomist and American surgeon can still claim some fame, Lewis Durlacher, a British podiatrist (surgeon chiropodist), had written a book on various foot ailments and described the foot this: ‘a kind of neuralgia seated between the toes, but which is not very common… the patient complains of pain between the second and third toes, generally the second and third, they can seldom tell.’ (Pastides, 2012).
The partial removal of the toe in 1997 was repaired without drama and constituted one of the most satisfactory if not complete neuroma excisions ever performed in my hands. The decision to not inform the patient and allow the outcome of course troubled me, but it turned out well. Fortunately, the patient was both young and had a good circulation
Citing backstory might make us sound erudite, but we fail to appreciate that the story can tell us so much more. For example, the neuralgic ganglion was similar in 1835 to my own experience and a nerve becomes distorted with expansion. Any credence to the term benign tumour, of which it is not, is but degeneration of a peripheral nerve with expansion. Sunderland (1953) classifies neuroma as type 4 as being a nerve injury that is not manageable except with surgery.
A bursa can coincide in the metatarsal spaces but confused the clinical and radiological signs. Durlacher defined intermetatarsal space 2, i.e. between the 2nd and 3rd; Morton defined the 4th MTPJ. He obsessed with metatarsals and trauma interspersed with neuralgia. The telling aspect of Durlacher’s description was that ‘they can seldom tell’. This is a critical observation of the diagnosis. It related to my case history in 1997 when the end of the toe appeared affected more than the space.
Durlacher and Morton are the only primary contenders for identifying the location. We could take any number of papers and establish a frequency in one location or another. Raouf (2019) assessed 1.6% in the first and 2.6% in the 4-5th intermetatarsal space. Many consider the other spaces void or never seen. True neuromata outside the 2nd and 3rdspaces are rare.
The table shows papers from different countries and sources with a bias overall toward the 3rdspace being more common than the 2nd space. Mean = 61.4/33.8% respectively. This suggests at least a 2:1 general chance. Ipsilateral and multi-space lesions arise but less frequently. The 4th interface arises between 1-8% of the time but the 1st space may not even be a neuroma. Bursa causing symptoms with a damaged nerve arose in 9% of my own cases taken from 91 histology reports. 13% of those reported had mixed neuroma and bursae. Bilateral neuroma exists around in approximately 25% of cases.
| First author | year | source | second space | third space |
| Bencardino | 2000, USA | radiology | 36 | 58 |
| Hewitt | 2006, UK | podiatry | 14 | 86 |
| Mahadevan | 2015, UK | orthopaedics | 38 | 34 |
| Naraghi | 2017, Au | podiatry | 42 | 38 |
| Raouf | 2019, USA | orthopaedics | 39 | 57 |
Digital Neuritis
Axonal mechanical sensitivities
We find amidst all the symptoms that paraesthesia is common, but pain can radiate to the ankle and even to the knee. Nerves don’t just form a neuroma, a thickened, scared and ischaemic nerve which forms a large fatty filled diameter around the nerve (see figure opposite). Neuritis can exist without nerve damage but can still experience strange sensations.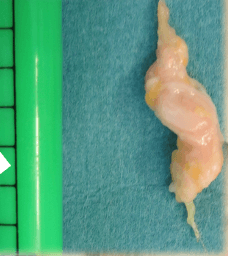
Satkeviciute (2018) highlights the effect of neuritis on axonal transport disruption without nerve injury. Citing from other sources, Satkevicuite suggests afferent nociceptor activity contributes to spontaneous pain and mechanically evoked radiating pain is recognised without nerve injury. This contributes to the observation of bizarre pain distribution pathways. Although outside this discussion, such activity is reputed to drive central mechanisms that cause hypersensitivity. Faster axonal transport brought about by inflammatory cellular activity at the site hyperpolarise-activate channels
Such is the curious aspect of anatomy that we call it neuralgia, for neuralgic pain, is doubtless one of the worst forms of pain because it alludes to satisfaction for many clinicians. As a patient, the first inkling of signs came from paraesthesiae; not due to a sudden onset but incipient changes that were random in many ways until the frequency crept in. This latent stage is easy to miss during the early stages.
Symptoms
Agreement between most papers list radiating pain, pebble or stone sensation in the shoe, numbness in the toe, cramp. The quality of pain includes sharp, stabbing, burning, ache as well as altered sensation. Rest and night pains are of more concern, and I confess the latter is real but hopefully short-lived and infrequent in my case. Relief in removing shoes is pathognomic of the neuroma.
Case histories from Morton
Morton’s 15 cases make interesting reading – how they arose and what patients thought, let alone expected. One was happy to have her leg amputated. The intensity of suffering for some led to the use of morphia. Removal of socks and shoes, treading on stones that cropped up, or twisting of the foot was part of Morton’s narrative. Confusion with gout was expressed and the duration extended to several decades of discomfort. In the case of my neuroma (2009-2016), I persevered for 7 years. Patients will present late to their doctors or podiatrists.
| Trauma – injury | Unstated | shoewear |
| 8 | 3 | 4 |
Most clinical papers will provide a similar story. Based on a sense of consistency (sensitivity) delineates that which suggests strongly that a digital nerve has been affected.
Mahedevan (2015) looked at the use of clinical tests numbering 7 and their sensitivity and specificity. These are two mathematical terms relating to the positive and negative incidence of findings, respectively. Of the two key radiological techniques used to validate the presence of a neuroma, Mahadevan used ultrasound. Looking at the picture of accurate determination from clinical examination, the following results were noted. Percussion and sensory have been combined as the least sensitive
| Clinical Test | Sensitivity (specificity) |
| Thumb/forefinger squeeze | 96% (96%) |
| Mulder’s click | 62% (62%) |
| Lateral compression of metatarsals | 41% (41%) |
| Percussion (dorsal & plantar) | 31% |
| Sensory (light & pinprick) | 25% |
This might not be the complete story. More responses arose with the thumb and forefinger because it is easier to achieve early sensory discomfort. Mulder’s click can only work if the lesion (neuroma) is large enough. Compression is similar and relies on more damage. The latter two are less sensitive but probably are more likely to yield results when the neuroma is at its worse. Mahadevan did not record any difference from pathological findings.
The quality of published papers
Branching out
Bencardino (2000) introduces the word ‘clinically silent’ based on the fact that not all neuromata are symptomatic. The does complicate the interpretation but one must assume as these were not removed no pathology could advise us except that the patients had not irritated the nerve to the extent of symptoms.
As far as aetiology is concerned we must be aware that there are variants of anatomy with 72% having no communicating branch between the lateral and medial plantar nerves and 28% having a connection (Govsa, 2005). The communicating branches were measured at around 1/2th thickness of the efferent nerve supplying the toes.
We are left with why the junction box 3-4th space experiences pain when in fact type III and IV patterns of branching include a 4-5th junction toe box connection. Symptoms might well arise in the 3-4th space more commonly because the mechanics and axes around the central metatarsals are different to the independent fifth metatarsal. If we return to Morton’s paper he states – “There is a slight lateral motion in the first three metatarsal bones, on account of their peculiar tarsal articulations; this is not so with the fourth and fifth, which have greater mobility, the fifth considerably more than the fourth…” One is reminded this was 1876 and was embellished in Root, Orien and Weed’s book in biomechanics a century later. The value of Govsa’s paper cannot be ruled out in regard to cause and frequency.
We see 2/3rd interspace or space 2 being affected but without a connecting branch. Again we can only rationalise this to combined foot deformity with hallux abducto-valgus and hammer toes distorting the anatomy as well as irritating any anatomical bursa.
Modern papers are just ‘window show.
Nineteenth-century papers are very different to those produced today. Papers were written in a particular language that reflected observation and hypothesis. Today scientific papers have a set style abstract, introduction (our back story), method, results, conclusion and discussion with a deposit of references usually bulked up with some minor works that are seldom relevant and may suggest a bibliographic citation. These references are window dressing and add no value to the narrative.
The modern meta-analysis applied to research processes and synthesisation was first introduced in the 1970s (Gurevitch et al. 2018). The citations in this paper give reference to much earlier thoughts on how data evolved. The cross-over from case history (CxH) to scientific evaluation bears close partnership because the CxH leads to the scientific question in the first place. Older papers, and indeed I include my own, were not always prospective, nor did they involve random constituent controls.
It is difficult to accept the material in one paper if it is not validated against another. For the Civinini-Morton neuroma, we cannot exclude Durlacher because together, for 41 years, the full knowledge was not revealed. Hoadley (1893) revealed a common combined condition called metatarsalgia. Hoadley operated through the sole in what Aydinlar (2014) believes was the first known surgical removal of a neuroma. This is misleading as Morton operated and described
‘after etherization, I made a longer incision than in the other operations, on the upper and outer side of the fourth metatarsal…’ 1876
He does go on to say he (Morton) divided the bone and removed the proximal phalanx, which one might say that had I indeed amputated the toe in my case, this would have appeared as radical as Morton! One of the conundrums that exist for any condition is that there will be a repository of information on PDN in the non-English speaking parts of the world. A failure to record, let alone publish, leads to the logical conclusion that many medical diagnoses might have come to light earlier but, of course, would be missed through lack of publication. Social media can be both a boon because of the speed of new information delivery but often challenged by lacking robustness, failing to be prospective, or having randomised controls, let alone ethical permission. Case histories have value as they sow seeds but fail in that they lack validation, observation and testing by impartial groups.
Accurate measurement
For the modern clinician, there are numerous methods of measuring pain in different circumstances. As with good research, exclusions must be rigorously applied so as not to confound data. Tools are another name for questionnaires and often attract scores to attain qualitative values.
The visual analogue scale (VAS), AOFAS score system for the forefoot, Manchester Pain Questionnaire, The Johnson Functional scale (satisfaction) and EQ-5D score sheets rank among methods to make a judgement that avoids bias and reduced objectivity. When someone else analyses the data without knowledge of the objectivity of the subject, an objective conclusion arises and bias reduces. For the purist, older papers tend to be poorly conceived and constructed than modern papers and would not pass a review committee.
Audit is another tool but often provides raw data and acts as a bean counter. This can suffer from the concept of retrospective analysis unless data is captured prospectively.
What else can we learn from backstories in the case of Morton’s neuroma?
Morton’s surgery was crude and inexact. Neuralgia meaning nerve pain was applied liberally to conditions often unknown but fitted the medical labelling to satisfy those who felt this important. Mislabelling still exists in medicine and attracts public following and a quest for such eponyms.
Gender, age and distribution
Mak (2021) uses the phrase ‘intermetatarsal neuropathy is a common forefoot pain’ in their opening sentence. Morton’s opening words in his 1976 paper were:
“During the past few years, I have had under my care a number of cases of a peculiar and painful affection, which, as far as I am aware, has not been described.”
Durlacher believed his 2-3rd space neuralgia was not common. Eleven of Morton’s 12 cited cases were female. As a crude statistic, this suggests a 91% gender bias. The age range ran from 20 – 50 for seven cases admitting age, giving a mean age of 34 or 32. So we learn from Morton that his group, albeit small in number, leaned toward a younger female patient.
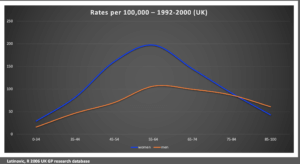
Latinovic (2006) provides the only robust data from the UK taken from the UK General Practice Research base with a cohort of 1.83 million patients. PASCOM-10 has, as of 2021 (October), collected 150,617 patients. Looking at data from 1/1/18 – 22/10/21, from 19,214 episodes of care, 1152 (6%) of patients were diagnosed with PDN.
Naraghi (2014) found data from the Australian Institute of Health and Welfare online database. Between 1998-2008 there were 13,579 admissions for Morton’s metatarsalgia. This ranged from 4.01 to 7.43 per 100,000 using the resident population to make the calculation. Latinovic cites data for PDN as 88/100,000 for females and 50/100,000 for males. Three per cent required surgery in 2000. If we compare Mahadevan 2015 and Bennett 1995, the conversion to surgery reached 10-20%+. Females present from 3 to 10 times more frequently with neuroma problems, and the GP database data is likely to understate the problem.
Medical care of patients was improving with more scrutiny for the minor afflictions over the gross injuries seen. In Morton’s case, during the American Civil War (1861-65), the crude amputations and swift decisions would have retained a sense of overkill and it would take years before surgery was refined. In 1893 Hoadley undertook a plantar incision for the nerve. As we progress with the advent of sensitive methods of identifying pathology, we will improve our approach to dealing with PDN. But we are left with one question to overcome, despite 150 years since Thomas G Morton and nearly 2 centuries since Civinini muted a lesion of the sole; what is the best algorithm for PDN if indeed one exists.
Continue reading about plantar digital neuroma
Digital Neuroma Old Problem New Analysis
![]()
A full list of references is available here
Thanks for reading ‘Metatarsalgia and the Foot Neuroma’ by David R Tollafield
Available through Amazon book as an ebook and paperback
Sign-up for here my regular FREE newsfeed
Published by Busypencilcase Communications. Est. 2015 for ConsultingFootPain



Recent Comments