A mysterious heel bump (Part 2)
‘Haglund’s deformity’
Let me try to demystify one type of heel pain known simply as the pump bump. Patients often ask how does a heel bump it arise and what we can do about my heel bump? Vaishya (2016) calls it a ‘common but mysterious condition’ in his paper . The reader needs to be aware that heel bump is a simplification and has some complex names. There are plenty of reasons for heel pain and this is one.
The retro calcaneal exostosis or Haglund’s deformity sound mysterious. Haglund as a name for a heel condition was so called after the man who described the problem in 1927.
I have this heel condition myself. My problem has been with me for thirty years. It was not until I was in my late forties that I experienced problems. My main concern was whilst driving, then latterly when wearing some designs of shoes. This has made me more aware of the design of my shoe. Pressure from the floor of the car stung my foot like crazy because my heel rubbed the skin while the foot was against the floor of the car. There were times when some shoes could rub the skin forming a blister. Reading score = 64
What is it?
When studying to become podiatrists, we called these heel bumps an exostosis or Haglund’s. The condition is not a disease but a deformity of the back of the heel bone (calcaneus). The term syndrome suggests that there is more than one condition. Those who read my articles regularly know I try to keep descriptions as simple as possible. Here is Vaishya’s complicated reasoning about the condition, but I will explain all the jargon after his paragraph.
Haglund’s deformity is an abnormality of the posterosuperior part of the calcaneus, where there is a bony enlargement at the attachment of the Achilles tendon. The adjoining soft tissues can irritate when this bony lump rubs against rigid shoes. It often leads to retrocalcaneal bursitis, calcaneal tendon bursitis, and thickening and inflammation of the calcaneal tendon. This combination of pathology is known as Haglund’s syndrome. Inflammation of the different parts of soft tissue in the area can lead to an isolated condition; however, the treatment options are different in these conditions, so they should be differentiated.
It can do so in three ways.
How is it caused?
Idiopathic means we don’t know or that the condition occurs without a clear reason. Poor-fitting of shoes is often due to the fact that the shoe does not suit the foot with a heel bump.
 Runners only experience this problem because they increase friction during running. This does not happen to runners only.
Runners only experience this problem because they increase friction during running. This does not happen to runners only.
Altered Biomechanics
While this label makes sense to podiatrists to the average man on the street, the word is just gobbledegook! Throw in the anatomical label, such as the subtalar joint (Fig.2), and this might confuse most people. This just means the lower half of the ankle joint. Let me describe the process in simple language.
The skin rubs against the shoe, but deeper pressure changes the thickness of the bone lining (periosteum). The periosteum adapts by laying down more bone. This arises where pressure and stress are greatest. This video makes for good education for those with a fascination for biology. The process of adapting bone is well-known and is called Wolff’s law. But what starts it off? Back to that word BIO-mechanics.
Mechanics
Mechanics implies the way things work or function according to physical principles. The foot is a wonder of mechanics. As it is living and biological, we call the movement and function ‘biomechanics’. As the heel contacts the ground, it rotates sideways, making contact with the inside lining of the shoe. This movement is called eversion and inversion, so in reality, tipping motions. This movement happens at one key joint. This is the subtalar joint. The forty-eight-second video will be helpful in understanding ankle movements. You can tell if this is a long-standing problem because the bone wears a small hole in the lining of the shoe.
If there is too much movement between the foot and the shoe, then the skin builds up friction (Fig.1). The foot moves in other directions, such as up and down at the true ankle joint (Fig. 2). Compression of the skin and deeper parts distort and set up shearing. Shearing forces are made from both friction (C) and compression (D) and create deep damage.
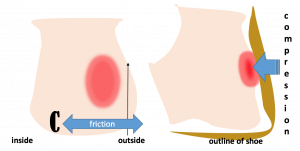
Figure 1 two views of the heel (left back, right side view). Area of skin stress shown in red.
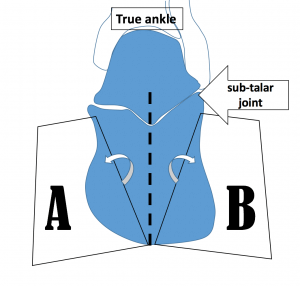
Figure 2. The subtalar joint is shown and pivots sideways toward A (eversion) or toward B (inversion) during walking. If the movement across both positions increases excessively, the deeper frictional forces cause shearing across the soft parts which become inflamed.
What can we do about your heel bump?
The first consideration is to manage any broken skin (acute injury). Prevention is better and so awareness of the shoe, your foot deformity and the surrounding terrain becomes a useful formula.

Haglund’s ‘syndrome’ suggests (1) the skin might be irritated or that (2) a deep bursa has become inflamed. This might have developed with some (3) tendon involvement. All three components might be present, but often it is only the bump that causes soreness. If it is simply the communal garden swelling, conservative management can be achieved by altering the heel height in shoe wear or using local protection.
The aim of any self-help management is to prevent blistering from arising or the skin from breaking and forming a ‘wound’. For anyone with neuropathy DO NOTE that damage can arise without immediate knowledge. Naturally, this has greater concern for patients with diabetes who suffer from numbness or neuropathy.

Gel sleeve is made from a thin elastic stocking with a thin spongy pad formed into the sock, as shown.
Acute
Direct skin pressure can be alleviated using a blister patch, but these should be used when acutely inflamed or where the skin has broken. Blister patches are sold in local pharmacies and chemist outlets.
A wound dressing will help absorb any leaking fluid to prevent infection. Change this regularly until any fluid leakage has stopped. Leave open to air at night so the foot does not stick to the sheets. Place a soft pillow or reposition yourself at night at the back of the leg (above the heel) to take pressure away from the raw skin.
Use a fresh dry dressing during the day. Avoid any further pressure and reduced the use of dressings unless necessary. Footwear such as flip flops, sandals or Crocs will help limit skin pressure while the skin mends. Pain medication is not required unless the level of pain is high, in which case if this is sustained for more than 2 days, seek help from a professional—normal pain medicines for headaches work. Try not to burst the roof of any blister unless it has become so large it will burst with footwear pressure. To burst a blister, you must use a clean technique. Using a standard antiseptic dressing is better than the recommendations to use Vaseline and is certainly preferred to antibiotic creams. As a rule, ointments should not be used on open wounds. There are always exceptions.
Prevention
The use of a siliconised gel sleeve, as shown in the picture above, is highly effective, and I have used this for walks when shoes that I know cause me problems despite fitting well enough. A felt pad cut out stuck to the inside of the shoe is helpful. This is often called a doughnut pad and is similar to the bunion pad I have demonstrated as part of my self-help videos.
New blister patch

PelliTec(R)
Adhering anything stick to the foot can damage the skin.
One of the problems with sticking anything to the skin is that the skin will become damaged in a short time. A recent pad that I have trialled is the ‘Pellitec blister patch. This can be stuck to the shoe in the same way felt can be applied. The pad is small and takes up little room, but it must be placed correctly. Measuring around 4.5cm in diameter, it should not be stuck to the skin. Mike McColgan has written about this in a recent article for ConsultingFootPain.
Initially, I had difficulty fitting the pad inside the heel of my walking boot. The area pressed, and the foam layer flattened. After a little trial and error, the pad worked and has stayed in place and, curiously, has not flattened out after 6 weeks. As my walking increased during the period of lockdown in March-May 2020, I must have walked a good 50 miles with my new blister pad and had no problem. My trusty boots had just become even more comfortable. I have eradicated all shoes from causing pressure on my heel to date.
Surgery
Most of the formal professional sites I have recommended all say something about surgery. This is not always a successful operation for large bumps. Smaller bumps, like mine, would work well enough if operated on. Recovery time is longer than you may realise; no less than 6 weeks and sometimes longer. Surgery is not for the faint-hearted, and the inconvenience is more to do with inconvenience than any lack of success. The usual risks exist, but this is where most sites do offer detailed information. As Vaishya suggests, ‘surgical excision of the bony exostoses of the calcaneum is only required in resistant cases.’ His further advice is also valid.
‘Inflammation of the different parts of soft tissue in the area can lead to an isolated condition; however, the treatment options are different in these conditions, so they should be differentiated.’
This condition can affect one or both heels. A history of arthritic conditions such as gout, rheumatoid arthritis, or seronegative spondyloarthropathies should be considered (Vaishya).
ConsultingFoot Pain says the best source at the time of publication was ACFS and FootEducation.

Fig.3 Courtesy College of Podiatry (open access) shows callus formation. The bump is toward the outside of the foot, as in Fig. 1
The American College of Foot Surgeons (good ***) has produced a useful overall impression, as does my usual site FootEducation (good***) which also uses the term ‘pump bump’. The British Foot and Ankle Society (poor*) does not talk about this condition within its brief discussion about heel pain. At the same time, the Royal College of Podiatry makes a brief statement (see box), but the RCP link seems to have disappeared at last checking!
|
Some people develop bumps on the back of the heel, often referred to as “pump bumps”. These are often a combination of local skin thickening, bursa and enlargement of the heel bone. This condition requires very careful investigation to determine the extent of the bump and whether there is any bone formed within the tendon. Depending on where the bump is and what structures are involved, treatment can sometimes be very difficult. Surgery is often associated with prolonged recovery and persistent swelling. Royal College of Podiatry |
Vaishya,R, Agarwal,AK, Azizi,AT, Vijay,V. Haglund’s Syndrome: A Commonly Seen Mysterious Condition. Oct; 8(10): e820. Published online 2016 Oct 7. doi: 10.7759/cureus.820
Thank you for reading a mysterious heel pain that follows my own journey by David Tollafield.
Updated last May 2021
David was a former Consultant Podiatric (foot) Surgeon and operated on many patients with the condition described in men and women, young and older adults, as well as having a Haglund’s deformity himself. He advocates conservative care wherever possible. His books include patient journeys, including another type of bump – Bunion Hallux valgus behind the scenes

Published by Busypencilcase Communications Ltd Est. 2015
Updated 23 June 2023


Recent Comments